Abstract
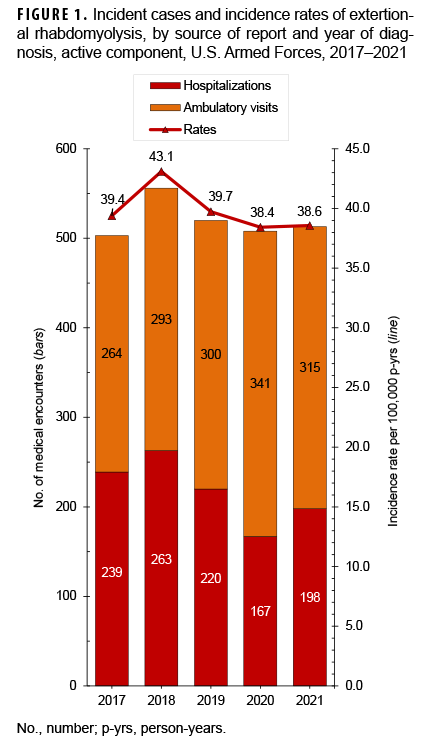
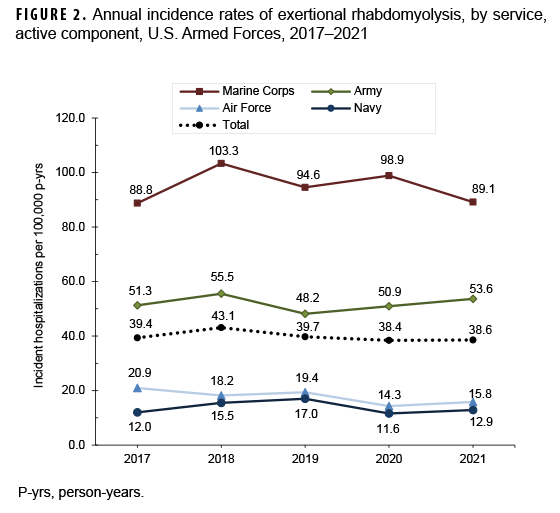
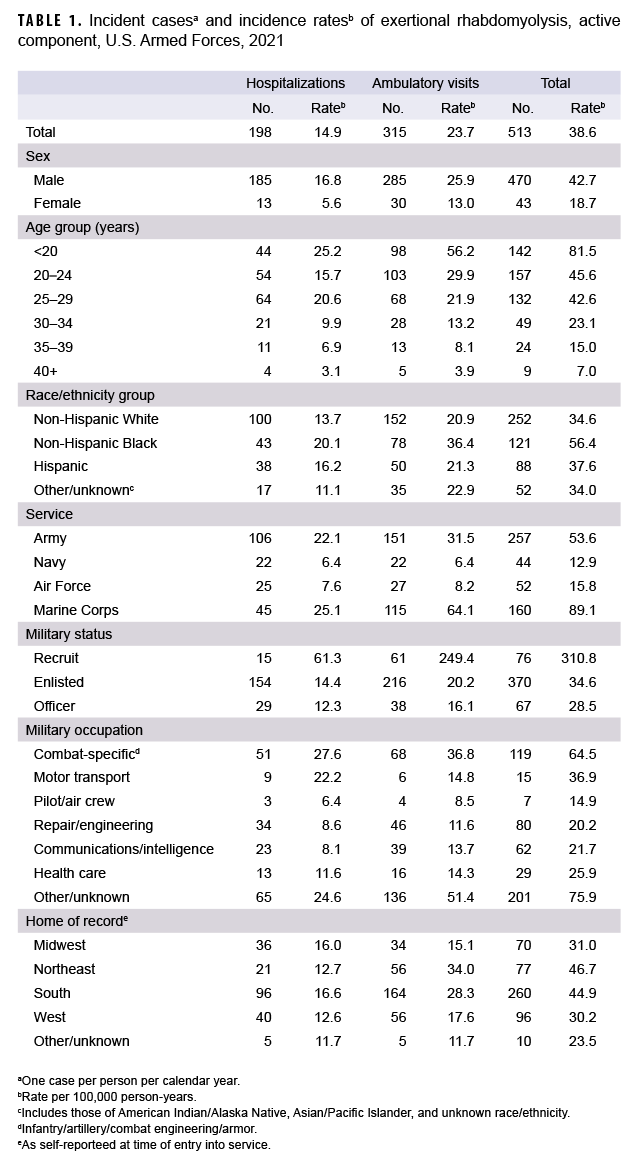
Among active component service members in 2021, there were 513 incident cases of exertional rhabdomyolysis, for an unadjusted incidence rate of 38.6 cases per 100,000 person-years (p-yrs). Subgroup-specific rates in 2021 were highest among males, those less than 20 years old, non-Hispanic Black service members, Marine Corps or Army members, recruits, and those in “other” and combat-specific occupations. During 2017–2021, crude rates of exertional rhabdomyolysis reached a peak of 43.1 per 100,000 p-yrs in 2018 after which the rate decreased to 38.4 and 38.6 per 100,000 p-yrs in 2020 and 2021, respectively. Compared to those in other race/ethnicity groups, non-Hispanic Black service members had the highest overall rate of exertional rhabdomyolysis in every year of the period. Overall and annual rates were highest among Marine Corps members, intermediate among those in the Army, and lowest among those in the Air Force and Navy. Most cases of exertional rhabdomyolysis were diagnosed at installations that support basic combat/recruit training or major ground combat units of the Army or the Marine Corps. Medical care providers should consider exertional rhabdomyolysis in the differential diagnosis when service members (particularly recruits) present with muscular pain or swelling, limited range of motion, or the excretion of darkened urine after strenuous physical activity, especially in hot, humid weather.
What are the new findings?
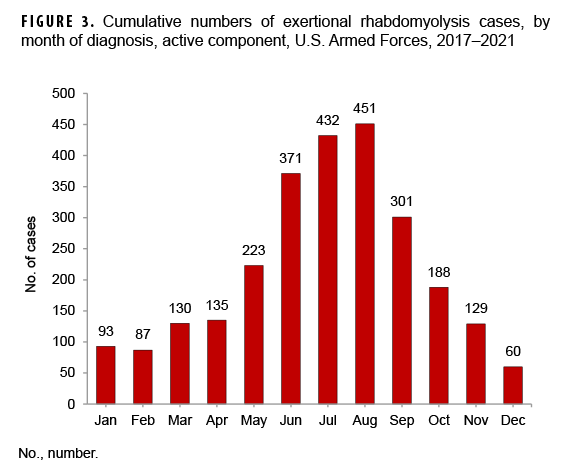
The 513 incident cases of exertional rhabdomyolysis in 2021 represented an unadjusted annual incidence rate of 38.6 cases per 100,000 p-yrs among active component service members, the second lowest during 2017–2021. Exertional rhabdomyolysis continued to occur most frequently from mid spring through early fall at installations that support basic combat/recruit training or major Army or Marine Corps combat units.
What is the impact on readiness and force health protection?
Exertional rhabdomyolysis is a potentially serious condition that requires a vigilant and aggressive approach. Some service members who experience exertional rhabdomyolysis may be at risk for recurrences, which may limit their military effectiveness and potentially predispose them to serious injury. The risk of exertional rhabdomyolysis can be reduced by taking into account fitness level, emphasizing graded, individual preconditioning before starting more strenuous training, and adhering to recommended work/rest ratios and hydration schedules, especially in hot, humid weather.
Background
Rhabdomyolysis is characterized by the breakdown of skeletal muscle cells and the subsequent release of intracellular muscle contents into the circulation. The characteristic triad of rhabdomyolysis includes weakness, myalgias, and red to brown urine (due to myoglobinuria) accompanied by an elevated serum concentration of creatine kinase.1,2 In exertional rhabdomyolysis, damage to skeletal muscle is generally caused by high-intensity, protracted, or repetitive physical activity, usually after engaging in unaccustomed strenuous exercise (especially with eccentric and/or muscle-lengthening contractions).3 Even athletes who are used to intense training and who are being carefully monitored are at risk of this condition,4 especially if new overexertion-inducing exercises are being introduced.5 Illness severity ranges from elevated serum muscle enzyme levels without clinical symptoms to life-threatening disease associated with extreme enzyme elevations, electrolyte imbalances, altered mental status, acute kidney failure, disseminated intravascular coagulation, compartment syndrome, cardiac arrhythmia, and liver dysfunction.1–3,6 A diagnosis of exertional rhabdomyolysis should be made when there are severe muscle symptoms (e.g., pain, stiffness, and/or weakness) and laboratory results indicating myonecrosis (usually defined as a serum creatine kinase level 5 or more times the upper limit of normal) in the context of recent exercise.7
Risk factors for exertional rhabdomyolysis include exertion in hot, humid conditions; younger age; male sex; a lower level of physical fitness; a prior heat illness; impaired sweating; and a lower level of education.1,3,8–11 Acute kidney injury, due to an excessive concentration of free myoglobin in the urine accompanied by volume depletion, renal tubular obstruction, and renal ischemia, represents a serious complication of rhabdomyolysis.6,12
In U.S. military members, rhabdomyolysis is a significant threat during physical exertion, particularly under heat stress.7,8,10,13 Moreover, although rhabdomyolysis can affect any service member, new recruits, who are not yet accustomed to the physical exertion required of basic training, may be at particular risk.10 Each year, the MSMR summarizes the numbers, rates, trends, risk factors, and locations of occurrences of exertional heat injuries, including exertional rhabdomyolysis. This report includes the data for 2017–2021. Additional information about the definition, causes, and prevention of exertional rhabdomyolysis can be found in previous issues of the MSMR.13
Methods
The surveillance period was January 2017 through December 2021. The surveillance population included all individuals who served in the active component of the Army, Navy, Air Force, or Marine Corps at any time during the surveillance period. All data used to determine incident exertional rhabdomyolysis diagnoses were derived from records routinely maintained in the Defense Medical Surveillance System (DMSS). These records document both ambulatory encounters and hospitalizations of active component members of the U.S. Armed Forces in fixed military and civilian (if reimbursed through the Military Health System [MHS]) treatment facilities worldwide. In-theater diagnoses of exertional rhabdomyolysis were identified from medical records of service members deployed to Southwest Asia/Middle East and whose healthcare encounters were documented in the Theater Medical Data Store.
For this analysis, a case of exertional rhabdomyolysis was defined as an individual with 1) a hospitalization or outpatient medical encounter with a diagnosis in any position of either “rhabdomyolysis” (International Classification of Diseases, 9th Revision [ICD-9]: 728.88; International Classification of Diseases, 10th Revision [ICD-10]: M62.82) or “myoglobinuria” (ICD-9: 791.3; ICD-10: R82.1) plus a diagnosis in any position of 1 of the following: “volume depletion (dehydration)” (ICD-9: 276.5*; ICD-10: E86.0, E86.1, E86.9), “effects of heat and light” (ICD-9: 992.0–992.9; ICD-10: T67.0*–T67.9*), “effects of thirst (deprivation of water)” (ICD-9: 994.3; ICD-10: T73.1*), “exhaustion due to exposure” (ICD-9: 994.4; ICD-10: T73.2*), or “exhaustion due to excessive exertion (overexertion)” (ICD-9: 994.5; ICD-10: T73.3*).13 Each individual could be considered an incident case of exertional rhabdomyolysis only once per calendar year. Incidence rates were calculated as incident cases of rhabdomyolysis per 100,000 person-years (p-yrs) of active component service. Percent change in incidence was calculated using unrounded rates.
To exclude cases of rhabdomyolysis that were secondary to traumatic injuries, intoxications, or adverse drug reactions, medical encounters with diagnoses in any position of “injury, poisoning, toxic effects” (ICD-9: 800.*–999.*; ICD-10: S00.*–T88.*, except the codes specific for “sprains and strains of joints and adjacent muscles” and “effects of heat, thirst, and exhaustion”) were not considered indicative of exertional rhabdomyolysis.14
For surveillance purposes, recruit trainees were identified as active component members who were assigned to service-specific training locations during the relevant basic training periods (e.g., 8 weeks for Navy basic training). Recruit trainees were considered a separate category of enlisted service members in summaries of rhabdomyolysis cases by military grade overall.
In-theater diagnoses of exertional rhabdomyolysis were analyzed separately; however, the same case-defining criteria and incidence rules were applied to identify incident cases. Records of medical evacuations from the U.S. Central Command (CENTCOM) area of responsibility (AOR) (i.e., Southwest Asia/Middle East) to a medical treatment facility outside the CENTCOM AOR also were analyzed separately. Evacuations were considered case defining if affected service members met the above criteria in a permanent military medical facility in the U.S. or Europe from 5 days before to 10 days after their evacuation dates.
It is important to note that medical data from sites that were using the new electronic health record for the Military Health System, MHS GENESIS, between July 2017 and October 2019 are not available in the DMSS. These sites include Naval Hospital Oak Harbor, Naval Hospital Bremerton, Air Force Medical Services Fairchild, and Madigan Army Medical Center. Therefore, medical encounter data for individuals seeking care at any of these facilities from July 2017 through October 2019 were not included in the current analysis.
Results
In 2021, there were 513 incident cases of rhabdomyolysis likely associated with physical exertion and/or heat stress (exertional rhabdomyolysis) (Table 1). The crude (unadjusted) incidence rate was 38.6 cases per 100,000 p-yrs. Subgroup-specific incidence rates of exertional rhabdomyolysis were highest among males (42.7 per 100,000 p-yrs), those less than 20 years old (81.5 per 100,000 p-yrs), non-Hispanic Black service members (56.4 per 100,000 p-yrs), Marine Corps or Army members (89.1 per 100,000 p-yrs and 53.6 per 100,000 p-yrs, respectively), and those in “other” and combat-specific occupations (75.9 and 64.5 per 100,000 p-yrs, respectively) (Table 1). Of note, the incidence rate among recruit trainees (310.8 per 100,000 p-yrs) was nearly 9 times the rates among other enlisted members and officers, even though cases among this group accounted for only 14.8% of all cases in 2021.
During the surveillance period, crude rates of exertional rhabdomyolysis reached a peak of 43.1 per 100,000 p-yrs in 2018 after which the rate decreased to 38.4 and 38.6 per 100,000 p-yrs in 2020 and 2021, respectively (Figure 1). The annual incidence rates of exertional rhabdomyolysis were highest among non-Hispanic Blacks during every year of the surveillance period; the rate among non-Hispanic Blacks decreased 16.8% from 67.9 per 100,000 p-yrs in 2017 to 56.4 per 100,000 p-years in 2021 (data not shown). Overall and annual rates of incident exertional rhabdomyolysis were highest among service members in the Marine Corps, intermediate among those in the Army, and lowest among those in the Air Force and Navy (Table 1, Figure 2). Among Marine Corps and Army members, annual rates increased in 2018, dropped in 2019, and then increased slightly in 2020 (Figure 2). In 2021, rates among Marine Corps members decreased while rates in Army members increased slightly. In contrast, annual rates among Air Force and Navy members were relatively stable between 2017 and 2021 but had decreased to their lowest points in 2020. During 2017–2021, approximately three-quarters (75.6%) of the cases occurred during the 6 months of May through October (Figure 3).
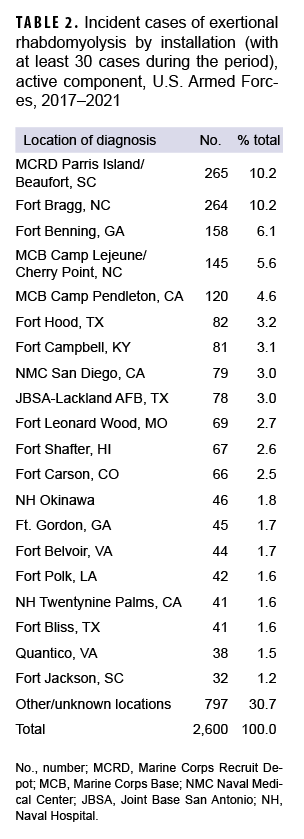
Rhabdomyolysis by location
During the 5-year surveillance period, the medical treatment facilities at 12 installations diagnosed at least 50 cases each; when combined, these installations diagnosed more than half (56.7%) of all cases (Table 2). Of these 12 installations, 4 provide support to recruit/basic combat training centers (Marine Corps Recruit Depot [MCRD] Parris Island/Beaufort, SC; Fort Benning, GA; Joint Base San Antonio-Lackland, TX; and Fort Leonard Wood, MO). In addition, 7 installations support large combat troop populations (Fort Bragg, NC; MCB Camp Lejeune/Cherry Point, NC; Marine Corps Base [MCB] Camp Pendleton, CA; Fort Hood, TX; Fort Shafter, HI; Fort Campbell, KY; Fort Carson, CO). During 2017–2021, the most cases overall were diagnosed at MCRD Parris Island/Beaufort, SC (n=265), and Fort Bragg, NC (n=264), which together accounted for about one-fifth (20.3%) of all cases (Table 2).
Rhabdomyolysis in the CENTCOM AOR
There were 7 incident cases of exertional rhabdomyolysis diagnosed and treated in the CENTCOM AOR (i.e., Southwest Asia/Middle East) (data not shown) during the 5-year surveillance period. Deployed service members who were most affected by exertional rhabdomyolysis were non-Hispanic Black or non-Hispanic White (n=4; 57.1% and n=3; 42.9%, respectively), male (n=5; 71.4%), 20–34 years old (n=6; 85.7%), in the Army (n=6; 85.7%), enlisted (n=6; 85.7%), and in health care occupations (n=3; 42.9%). One active component service member was medically evacuated from the CENTCOM AOR for exertional rhabdomyolysis during the surveillance period; this medical evacuation occurred in November 2020 (data not shown).
Editorial Content
This report documents that the crude rates of exertional rhabdomyolysis reached a peak of 43.1 per 100,000 p-yrs in 2018 after which the rates decreased to 38.4 and 38.6 per 100,000 p-yrs in 2020 and 2021, respectively (10%–11.0% decrease). Exertional rhabdomyolysis occurred most frequently from mid spring through early fall at installations that support basic combat/recruit training or major Army or Marine Corps combat units.
The risks of heat injuries, including exertional rhabdomyolysis, are elevated among individuals who suddenly increase overall levels of physical activity, recruits who are not physically fit when they begin training, and recruits from relatively cool and dry climates who may not be acclimated to the high heat and humidity at training camps in the summer.1,2,10 Soldiers and Marines in combat units often conduct rigorous unit physical training, personal fitness training, and field training exercises regardless of weather conditions. Thus, it is not surprising that recruit camps and installations with large ground combat units account for most of the cases of exertional rhabdomyolysis.
The annual incidence rates among non-Hispanic Black service members were higher than the rates among members of other race/ethnicity groups. This observation has been attributed, at least in part, to an increased risk of exertional rhabdomyolysis among individuals with sickle cell trait (SCT)15–18 and is supported by studies among U.S. service members.10,19,20 The rhabdomyolysis-related deaths of 2 SCT-positive service members (an Air Force member and a Navy recruit) after physical training in 2019 highlight this elevated risk.21,22 However, although it is well established that sickle cell trait is positively associated with exertional rhabdomyolysis, its association with disease progression and severity is unclear and warrants further study.19,20
The findings of this report should be interpreted with consideration of its limitations. A diagnosis of “rhabdomyolysis” alone does not indicate the cause. Ascertainment of the probable causes of cases of exertional rhabdomyolysis was attempted by using a combination of ICD-9/ICD-10 diagnostic codes related to rhabdomyolysis with additional codes indicative of the effects of exertion, heat, or dehydration. Moreover, other ICD-9/ICD-10 codes were used to exclude cases of rhabdomyolysis that may have been secondary to trauma, intoxication, or adverse drug reactions. In addition, recruit trainees were identified using an algorithm based on age, rank, location, and time in service. This method is only an approximation and likely resulted in some misclassification of recruit training status.
The measures that are effective at preventing exertional heat injuries in general apply to the prevention of exertional rhabdomyolysis. In the military training setting, the risk of exertional rhabdomyolysis can be reduced by emphasizing graded, individual preconditioning before starting a more strenuous exercise program and by adhering to recommended work/rest and hydration schedules, especially in hot weather. The physical activities of overweight and/or previously sedentary new recruits should be closely monitored. Strenuous activities during relatively cool mornings following days of high heat stress should be particularly closely monitored; in the past, such situations have been associated with increased risk of exertional heat injuries (including rhabdomyolysis).8
Management after treatment for exertional rhabdomyolysis, including the decision to return to physical activity and duty, is a persistent challenge among athletes and military members.10,11,23 It is recommended that those who have had a clinically confirmed exertional rhabdomyolysis event be further evaluated and risk stratified for recurrence before return to activity/duty.7,11,23,24 Low-risk patients may gradually return to normal activity levels, while those deemed high risk for recurrence will require further evaluative testing (e.g., genetic testing for myopathic disorders).23,24
Commanders and supervisors at all levels should ensure that guidelines to prevent heat injuries are consistently implemented, be vigilant for early signs of exertional heat injuries, and intervene aggressively when dangerous conditions, activities, or suspicious illnesses are detected.7 Finally, medical care providers should consider exertional rhabdomyolysis in the differential diagnosis when service members (particularly recruits) present with muscular pain or swelling, limited range of motion, or the excretion of darkened urine (possibly due to myoglobinuria) after strenuous physical activity, especially in hot, humid weather. The treatment of suspected and confirmed cases should be guided by the most current clinical practice guidelines.7
References
1. Zutt R, van der Kooi AJ, Linthorst GE, Wanders RJ, de Visser M. Rhabdomyolysis: review of the literature. Neuromuscul Disord. 2014;24(8):651–659.
2. Beyond muscle destruction: a systematic review of rhabdomyolysis for clinical practice. Chavez L, Leon M, Einav S, Varon J. Crit Care. 2016;20:135
3. Rawson ES, Clarkson PM, Tarnopolsky MA. Perspectives on exertional rhabdomyolysis. Sports Med. 2017;47(suppl 1):33–49.
4. McKewon S. Two Nebraska football players hospitalized, treated after offseason workout. Omaha World-Herald. 20 January 2019. Accessed 1 March 2022. https://www.omaha.com/huskers/football/two-nebraska-football-players-hospitalized-treated-after-offseason-workout/article_d5929674-53a7-5d90-803e-6b4e9205ee60.html
5. Raleigh MF, Barrett JP, Jones BD, Beutler AI, Deuster PA, O'Connor FG. A cluster of exertional rhabdomyolysis cases in a ROTC program engaged in an extreme exercise program. Mil Med. 2018;183(suppl 1):516–521.
6. Bosch X, Poch E, Grau JM. Rhabdomyolysis and acute kidney injury. N Engl J Med. 2009;361(1):62–72.
7. O’Connor FG, Deuster P, Leggit J, et al. Clinical Practice Guideline for the Management of Exertional Rhabdomyolysis in Warfighters 2020. Bethesda, Maryland: Uniformed Services University. 2020.
8. Hill OT, Wahi MM, Carter R, Kay AB, McKinnon CJ, Wallace RF. Rhabdomyolysis in the U.S. active duty Army, 2004–2006. Med Sci Sports Exerc. 2012;44(3):442–449.
9. Lee G. Exercise-induced rhabdomyolysis. R I Med J. 2014;97(11):22–24.
10. Hill OT, Scofield DE, Usedom J, et al. Risk factors for rhabdomyolysis in the U.S. Army. Mil Med. 2017;182(7):e1836–e1841.
11. Knapik JJ, O’Connor FG. Exertional rhabdomyolysis: epidemiology, diagnosis, treatment, and prevention. J Spec Oper Med. 2016;15(3):65–71.
12. Holt S, Moore K. Pathogenesis of renal failure in rhabdomyolysis: the role of myoglobin. Exp Nephrol. 2000;8(2):72–76.
13. Armed Forces Health Surveillance Branch. Update: Exertional rhabdomyolysis among active component members, U.S. Armed Forces, 2014–2018. MSMR. 2019;26(4):21–26.
14. Armed Forces Health Surveillance Branch. Surveillance case definition. Exertional rhabdomyolysis. Accessed 1 March 2022. https://www.health.mil/Reference-Center/Publications/2017/03/01/Rhabdomyolysis-Exertional
15. Gardner JW, Kark JA. Fatal rhabdomyolysis presenting as mild heat illness in military training. Mil Med. 1994;159(2):160–163.
16. Makaryus JN, Catanzaro JN, Katona KC. Exertional rhabdomyolysis and renal failure in patients with sickle cell trait: is it time to change our approach? Hematology. 2007;12(4):349–352.
17. Ferster K, Eichner ER. Exertional sickling deaths in Army recruits with sickle cell trait. Mil Med. 2012;177(1):56–59.
18. Naik RP, Smith-Whitley K, Hassell KL, et al. Clinical outcomes associated with sickle cell trait: a systematic review. Ann Intern Med. 2018;169(9):619–627.
19. Nelson DA, Deuster PA, Carter R, Hill OT, Wolcott VL, Kurina LM. Sickle cell trait, rhabdomyolysis, and mortality among U.S. Army soldiers. N Engl J Med. 2016;375(5):435–442.
20. Webber BJ, Nye NS, Covey CJ, et al. Exertional Rhabdomyolysis and Sickle Cell Trait Status in the U.S. Air Force, January 2009–December 2018. MSMR. 2021;28(1):15–19.
21. Air Combat Command. U.S. Air Force Ground Accident Investigation Board Report. 20th Component Maintenance Squadron 20th Fighter Wing, Shaw Air Force Base, South Carolina. Fitness assessment fatality; 24 May 2019.
22. Mabeus C. Autopsy reports reveal why two recruits died at boot camp. NavyTimes. 8 November 2019. Accessed 1 March 2022. https://www.health.mil/Reference-Center/Publications/2017/03/01/Rhabdomyolysis-Exertional
23. O’Connor FG, Brennan FH Jr, Campbell W, Heled Y, Deuster P. Return to physical activity after exertional rhabdomyolysis. Curr Sports Med Rep. 2008;7(6):328–331.
24. Atias D, Druyan A, Heled Y. Recurrent exertional rhabdomyolysis: coincidence, syndrome, or acquired myopathy? Curr Sports Med Rep. 2013;12(6):365–369.