What are the New Findings?
This study found that indirect medical costs (i.e., loss of return on personnel salary) cost the Army nearly 4 times the amount spent on direct medical care for soldiers' lower extremity fractures. This estimate assumes that lost duty time was equivalent to the number of days hospitalized for a lower extremity fracture and limited duty was equal to 120 days at 50% productivity for each lower extremity fracture. Study findings demonstrate the value of including indirect costs to obtain a comprehensive understanding of the financial burden of military injuries.
What Is the Impact on Readiness and Force Health Protection?
Injury costs estimates inform Army injury prevention initiatives and prioritization efforts. However, a standardized method for estimating Army injury costs is needed. The methodology developed for this analysis fills a critical gap in Army estimates of injury burden and provides the foundation for future expanded cost estimates.
Abstract
The estimated cost to the Army for lower extremity fractures in 2017 was approximately $116 million. Direct medical expenses totaled $24 million, and indirect medical costs totaled $92 million ($900 thousand lost duty; $91 million limited duty). Foot and toe fractures, along with lower leg and ankle fractures accounted for the majority of soldiers' initial visits for care (n=4,482; 91.6%), and more than $103 million (89.0%) of overall costs ($116 million). Costs varied by location of care. In outpatient settings, initial visits for foot and toe injuries accounted for the highest costs: $49 million overall. Direct medical costs totaled $1.2 million, and indirect medical costs (limited duty) were $48 million. Conversely, in inpatient settings, lower leg and ankle fractures accounted for slightly more than half of all costs (overall $9 million; $4.8 million in direct medical costs and $4.5 million in indirect medical costs). The finding that the majority of costs related to lower extremity fractures were due to estimated days of lost or limited duty and associated loss of productivity justifies the inclusion of indirect cost estimates as a part of overall injury cost calculations.
Background
Injuries have long been the leading challenge to the Army's ability to optimize medical readiness and soldier health.1–3 The likelihood of a soldier experiencing an injury is high, with over half of soldiers experiencing a new injury annually.4 Overall, there are over 1,800 new injuries diagnosed per 1,000 soldiers each year.4 Many of these injuries are preventable, lead to costly medical encounters and lost productivity among military personnel, and account for the status of more than half of all medically non-deployable Army soldiers.5-7
This analysis is centered on acute fractures of the lower extremities. Acute fractures are considered "severe" injuries due to the frequent need for hospitalization and the amount of recovery time required before a soldier can return to work at full capacity. U.S. Army surveillance data from 2015 indicate that 45% of acute injury hospitalizations were due to fractures.8 Prior studies have estimated the number of lost duty days attributed to fractures to range from 73 to 120 days—compared to 35 days for dislocations, 18 to 30 days for sprains and strains, and 3 to 11 days for heat- and cold-weather related injuries.9–11 The purpose of this study was to develop a standardized methodology for estimating the direct and indirect medical costs of military injuries. The analyses focused on lower extremity fractures, in particular, because such injuries are considered by both the Army safety and health communities to be a high-visibility, high priority concern.12,13 No papers to date have addressed the costs of fractures to the Army or to other military services.
Methods
Centering on factors of interest to the military (a military-societal perspective), a cost-of-illness approach was used to combine information on the number of injuries and the impact of their associated health care utilization into single estimates of cost.14–17 A cross sectional, prevalence based study design was employed. Therefore, all acute lower extremity fractures requiring medical care - both new and ongoing for calendar year (CY) 2017 - were included in the analysis. The resulting injury estimates provide the costs of lower extremity fractures in a single year, rather than recurrent costs of these injuries over the course of a soldier's career.
This study included injuries identified in the medical records from the active component of the U.S. Army. Army Reserve and National Guard members on active duty status at any time during CY 2017 were also included. These data represent injury-related care received in or paid for by the Military Health System (MHS) and were obtained from MHS Data Repository (MDR) files including the Standard Inpatient Data Record (SIDR) (military treatment facility [MTF] inpatient data), the Comprehensive Ambulatory/Professional Encounter Record (CAPER) (MTF outpatient data), TRICARE Encounter Data Institutional (TED-I) (inpatient data), and TED-Non-Institutional (NI) (records of outpatient purchased care) using the MHS Mart (M2) interface.
Lower extremity fractures were identified using International Classification of Disease, 10th Revision, Clinical Modification (ICD-10-CM) medical diagnostic codes. The listing of codes was identified using an ICD-10-CM Injury Mortality Diagnosis (IMD) Matrix.18 The inclusion criterion for a case was any medical encounter with an ICD-10 diagnosis code of S72 (fracture of bones in hip or upper leg), S82 (fracture of bones in the knee, lower leg, or ankle), or S92 (fracture of bones in the feet or toes) recorded in the first or second diagnostic position. All extenders for the listed codes were captured and included in the analysis.
Inclusion of the first 2 diagnosis code positions varies from the methodology used in previous incidence and prevalence studies of Army injuries, which limited inclusion criteria to the first diagnosis code position only. A review of several case examples found that many fractures were not identified by a primary diagnosis because a diagnosis of "pain" in a lower extremity often preceded the fracture diagnosis. It was necessary to use the secondary diagnosis to more completely capture all fractures and associated direct costs for treatments and indirect costs via estimated days of lost duty. A 365-day incidence rule was applied by person and injury in order to reduce the effect of follow-up injury visits and potential overestimation of frequencies and rates. The rule states that multiple visits for the same 3-digit ICD-10-CM diagnosis within 365 days of the initial visit were counted as only 1 visit, allowing only 1 injury of the same type per year.
Comprehensive cost-of-illness metrics—both direct and indirect costs—were examined. Direct medical cost was defined as the cost of care associated with the fracture encounter paid for by the MHS. All direct medical cost data were extracted from the MDR and were included for each injury encounter. Two types of indirect medical costs were determined: (1) lost duty time, in which a soldier is not able/ available to perform his/her duties due to health care (e.g., injury-related hospitalizations); and (2) limited duty time, in which a soldier either could not participate in his/her military occupational and physical training tasks and/or performed these tasks at diminished capacity due to the injury (e.g., working while injured). The amount of time lost (lost duty time) is based on hospital length of stay associated with a lower extremity fracture. Clinician visit duration or appointment time is not consistently captured across all outpatient settings. No assumptions were made for the length of time for visits and no lost duty time was estimated for time away from duties associated with these appointments. Given the incomplete capture of limited duty days in military medical records, the amount of limited time (limited duty days) for lower extremity fractures was based on estimates from existing literature.9
Data were extracted, downloaded, and analyzed using SAS/STAT software, version 9.4 (2014, SAS Institute, Cary, NC). Analyses of lower extremity fractures resulting in inpatient and outpatient treatment were stratified by body region and encounter type. The number of soldiers treated for lower extremity fractures (along with age, sex, and rank group characteristics), frequency of encounters, and estimated limited duty days were reported. Total cost was calculated as the sum of direct medical cost and indirect medical cost.
Direct medical cost, the full cost and/ or total amount paid for an injury encounter, was summed respectively for the three fracture diagnosis codes (based on ICD10 codes S72, S82, and S92). Data were reported in 2017 U.S. dollars by location of care (outpatient and inpatient) and by injury encounter type using available ICD10-CM extension digits. Initial encounters (first occurrence) were indicated by a seventh digit of "A", "B", or "C", followup encounters by "D" "R", and sequela encounters by "S".
Indirect medical cost, the costs associated with estimated lost duty time and limited duty time, were calculated by linking each soldier's rank from his/her initial encounter to military pay charts.19 The 2 types of indirect medical costs are considered independent and an injury could be associated with both lost duty time and limited duty time. Indirect medical cost associated with lost duty time for inpatient stays was calculated as the number of days spent in the hospital multiplied by the salary associated with the soldier's rank at the time of the injury. No lost duty time was calculated for outpatient visits. Indirect medical cost associated with limited duty time, based on Ruscio's estimate,9 was calculated only for the initial occurrence of each injury of interest.9 The first occurrence of a fracture with an initial encounter indicator (i.e., an "A", "B", or "C") in the seventh position of the ICD code was first assumed to result in 120 days of limited duty.9 Upon further consideration by injury subject matter experts, and to provide conservative estimates for this analysis, it was assumed that all 120 days were limited duty at 50% productivity. Therefore, the cost of 1 limited duty day was considered equal to half of a service member's daily pay. For 120 days of limited duty, the cost of an injury would equal 120 (days) x 50% of the soldier's daily salary.
Results
Table 1 shows there were 5,287 soldiers who experienced at least 1 lower extremity fracture in CY 2017 (83.3% men, 16.7% women). Over two-fifths (44.1%) of those with lower extremity fractures were 30 years of age or older and 44.0% were less than E-5 in rank. More than half (54.5%) of soldiers with lower extremity fractures experienced fractures to the foot and toes (n=2,880), and 37.1% experienced fractures to the lower leg and ankle (n=1,962); all other anatomical sites for the lower extremity accounted for the remaining 8.9% of fractures (n=445).
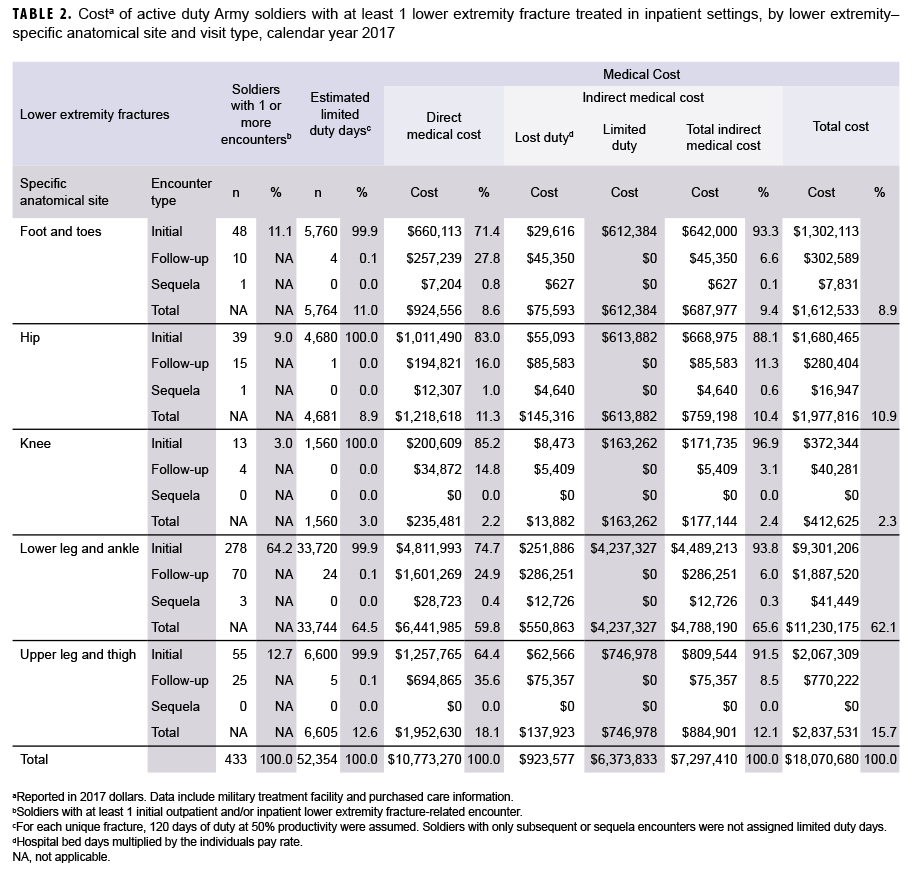
Cost of inpatient care for lower extremity fractures
A total of 433 soldiers received inpatient care for lower extremity fractures (Table 2). The number of soldiers hospitalized for lower leg and ankle fractures (n=278) was 5 times the number hospitalized for upper leg and thigh fractures (n=55), the second most common fracture location. Lower leg and ankle fractures accounted for the highest number of limited duty days associated with inpatient treatment (n=33,744; 64.5%). Lower leg and ankle fractures also accounted for the highest direct medical costs, just over $6.4 million (59.8% of total direct medical inpatient costs); the highest lost duty cost, slightly more than $550 thousand (59.6% of the cost associated with bed days); and the highest limited duty cost, about $4.2 million (66.4% of the cost associated with lost productivity). Of the estimated $18.1 million in inpatient cost reported in Table 2, $11.2 million (62.1%) was associated with lower leg and ankle fractures.
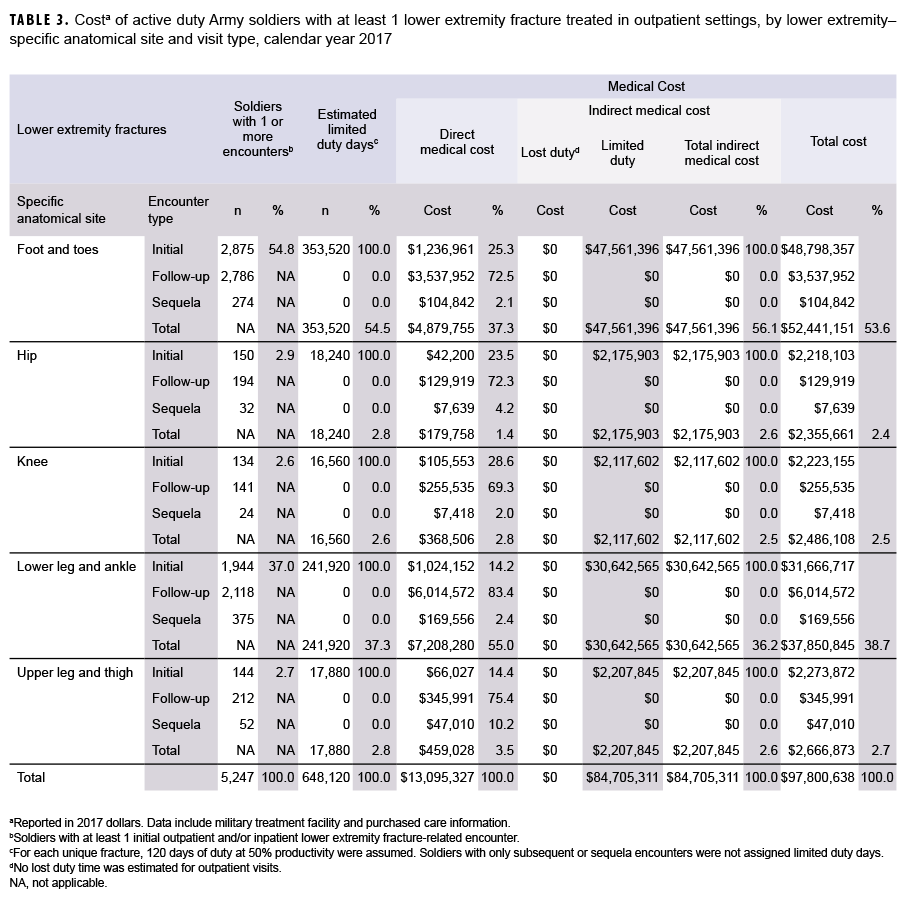
Cost of outpatient care for lower extremity fractures
Table 3 shows that 5,247 soldiers received outpatient care for lower extremity fractures. More soldiers made initial visits for foot and toe fractures (n=2,875; 54.8%) than for lower leg and ankle fractures (n=1,944; 37.0%). A smaller number of soldiers experienced lower extremity fractures in other anatomical sites (n=428; 8.2%).
The highest direct medical costs resulted from lower leg and ankle fractures ($7.2 million; 55.0%), followed by foot and toe fractures ($4.9 million; 37.3%). The highest indirect costs—lost or limited productivity costs due to limited duty time—resulted from foot and toe fractures ($47.6 million; 56.1%). Likewise, the highest total costs associated with outpatient encounters were for foot and toe fractures ($52.4 million; 53.6%), followed by lower leg and ankle fractures ($37.9 million; 38.7%).
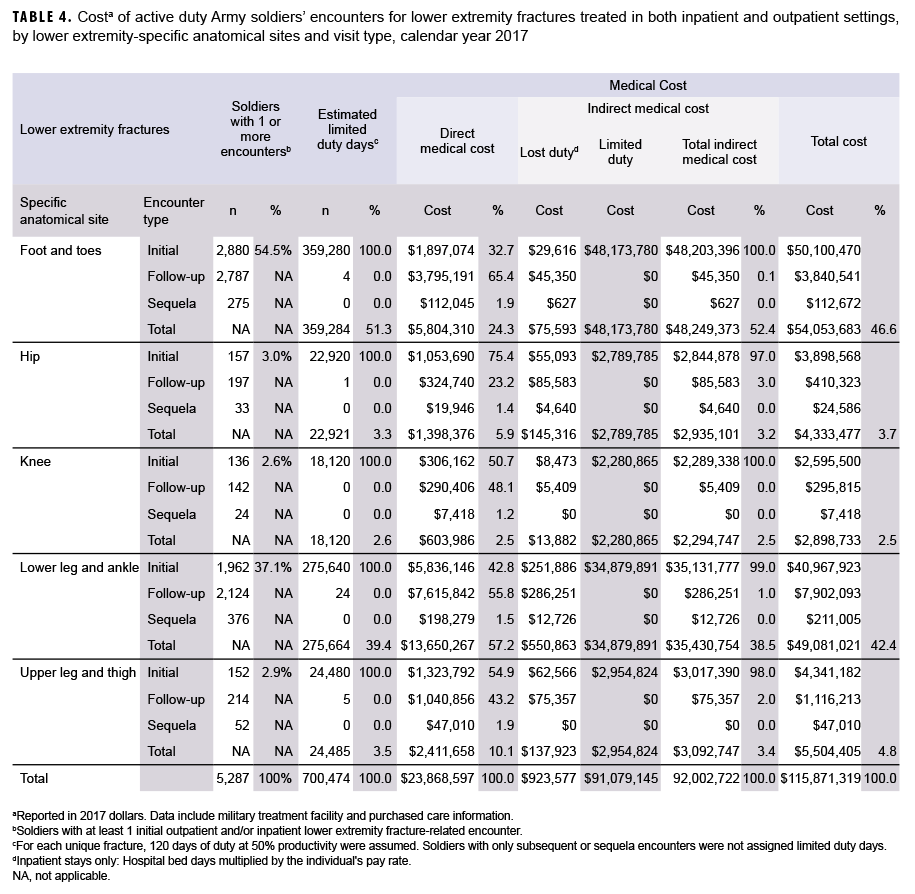
Cost of inpatient and outpatient care for lower extremity fractures
Table 4 shows that 5,287 soldiers received care for lower extremity fractures in inpatient and/or outpatient sites in CY 2017; 40 soldiers received care in an inpatient setting only (data not shown). More soldiers made initial visits for fractures of the foot and toe (n=2,880; 54.5%) than for fractures of the lower leg (n=1,962; 37.1%). Far fewer soldiers sought initial medical encounters for the other categories of lower extremity fracture (hip, n=157, 3.0%; upper leg and thigh, n= 152, 2.9%; knee, n=136, 2.6%).
Fractures to the foot and toes resulted in more days of limited duty than any other anatomical site of the lower extremities: 359,284 days (51.3% of the total days). The second greatest number of limited duty days was for lower leg and ankle fractures: 275,664 (39.4%) of the total days of limited duty.
The highest total costs for lower extremity fractures were associated with foot and toe fractures ($54.1 million; 46.6%), followed by the cost of lower leg and ankle fractures ($49.1 million; 42.4%). These 2 anatomical sites accounted for 89.0% of total costs.
Editorial Comments
In a single year (CY 2017), lower extremity fractures—the most common cause of hospitalization among military service members—cost the Army an estimated $116 million in direct and indirect medical cost, and more than 5,000 active duty soldiers experienced 1 or more lower extremity fractures in CY 2017. Even though lower extremity fractures are considered "serious" injuries, the largest percentage of associated costs ($97.8 million; 84.4%) was incurred by fractures treated in outpatient settings. Overall, 5,247 soldiers had outpatient encounters for lower extremity fractures. The majority of soldiers treated in outpatient settings for lower extremity fractures had encounters for fractures to foot and toes (54.8%), followed by fractures to lower leg and ankle (37.0%). Although more serious, the costs of lower extremity fractures requiring hospitalization were only $18.1 million, or 15.6% of the total costs. However, the costs per case for fractures treated in inpatient settings was 9 times the cost of those treated on an outpatient basis ($30,628 per case versus $3,370 per case [Encounter data reported in the full technical report21]). Among the 433 soldiers hospitalized for lower extremity fractures, 64.2% were hospitalized for fractures to lower legs and ankles, followed by upper leg and thigh fractures (12.7%). Overall, the indirect costs of fractures ($92.0 million) were approximately 4 times greater than costs associated with direct medical expenses ($23.9 million). These indirect costs were clearly driven by the cost associated with limited duty days ($91.1 million of the $92.0 million). This study estimated that more than 700,000 limited duty days were associated with lower extremity fractures in 2017; 648,000 days were related to soldiers treated in outpatient settings, and 52,000 days were related to soldiers who were hospitalized.
While the cost of fractures has not been previously reported, the diagnosis, distribution, and anatomical locations of these acute injuries for outpatient cases were similar to those seen previously among military service members.2 The distribution of lower extremity fractures treated in hospitals in this study was also similar to the distributions reported among service members2 and among medical evacuation cases during Operation Iraqi Freedom/Operation Enduring Freedom.20
This study estimated both direct and indirect medical costs attributed to a specific type of injury more precisely than any prior study. While days of lost duty and limited duty were estimated to determine the indirect costs, these costs were segregated by complete loss of duty time (such as due to hospital or bed restriction) and the cost of restricted abilities (represented as productivity loss). A study innovation involved inclusion of the secondary diagnosis in the case definition after study investigators noted a diagnosis of "pain" in a lower extremity often precedes the fracture diagnosis for these injuries. As a result, an additional 531 injuries of interest were appropriately identified. Methodological details are documented in an earlier APHC public health information paper.21
As an initial study, some limitations are acknowledged. Study estimates may overestimate costs associated with fractures where comorbid conditions (i.e., other injuries or conditions) contributed to the cost of the encounters. Additional analysis should be conducted to better understand the likelihood and magnitude of this concern. The basis for estimation of limited duty of 120 days was from information in the literature and not actual profile days assigned by providers, and therefore may lack precision. Additionally, these estimates are not differentiated by type of injury and could overestimate the cost for fractures where the number of limited duty days for a specific injury type were less than the estimated 120 days (e.g., toe fractures and metatarsal fractures). While the researchers addressed this concern by assuming that all 120 days were limited duty at 50% productivity; the productivity cutoff was based on the experience of injury prevention subject matter experts. Sensitivity analysis could be conducted to confirm the efficacy of this decision. The cost for fractures may be underestimated where visits preceding the fracture diagnosis (e.g., for pain) were not included in cost estimates. Appointment time is also lost duty time but was not available for all data sources and was not included in this analysis. Not all costs were captured since fractures recorded in diagnostic positions 3–10 were not included. Lower extremity fracture costs associated with outpatient surgeries (e.g., Current Procedural Terminology [CPT] codes 27600–27899, surgical procedures to the leg and ankle), may not have been captured especially where these costs were attached to visits preceding the fracture diagnosis. Costs for care paid by insurers outside the MHS as well as the cost for other care, such as informal care, were not included and are a source of underestimation as well.
Study findings support the methodological value of estimating Army injury costs. Specifically, the results demonstrate that the majority of costs of lower extremity fractures result from the indirect costs associated with limited duty time. This finding and the methods used to calculate the associated indirect and direct costs address a gap which has previously existed in the study and surveillance of military injuries.
Author affiliations: Injury Prevention Program, U.S. Army Public Health Center, Aberdeen Proving Ground, MD (COL Jones, Ms. Hauschild, Dr. Schuh-Renner, Mr. Grier, Ms. Dada, Dr. Canham-Chervak); U.S. Army Satellite, Armed Forces Health Surveillance Division, Public Health Division/Defense Health Agency (Dr. Forrest, Mr. Barnes, Mr. Steelman).
Disclaimer: The views expressed herein are those of the authors and do not necessarily reflect the official policy or position of the Army, the Department of Defense, or the U.S. Government.
References
- Nindl BC, Williams TJ, Deuster PA, et al. Strategies for optimizing military physical readiness and preventing musculoskeletal injuries in the 21st century. US Army Med Dep. 2013;J:5-23.
- Jones BH, Canham-Chervak M, Canada S, et al. Medical surveillance of injuries in the U.S. military descriptive epidemiology and recommendations for improvement. Am J Prev Med. 2010;38(1 Suppl):S42-60.
- National Research Council. Assessing fitness for military enlistment: physical, medical, and mental health standards. Washington, DC: National Academies Press; 2006.
- U.S. Army Public Health Center (APHC). Health of the Force Report 2018. Accessed 22 March 2019. https://phc.amedd.army.mil/Periodical%20Library/2018HealthoftheForceReport.pdf
- Shuping E, Canham-Chervak M, Amoroso PJ, et al. Identifying modifiable causes of fall-related injury: an analysis of U.S. Army safety data. Work. 2009;33:23-34.
- Army Public Health Center. Health of the Force Report 2017. Accessed 15 March 2019. https://phc.amedd.army.mil/Periodical%20Library/2017HealthoftheForceweb.pdf#search=2017%20health%20of%20the%20force
- National Safety Council. Department of Defense Executive Assessment of Safety and Occupational Health Management Systems. 6 December 2001.
- Army Public Health Center. U.S. Army Injury Surveillance Summary 2016. Accessed 23 August 2021. https://phc.amedd.army.mil/Periodical%20Library/USArmyInjurySurveillanceSummary2016.pdf
- Ruscio BA, Jones BH, Bullock SH, et al. A process to identify military injury prevention priorities based on injury type and limited duty days. Am J Prev Med. 2010;38(1 Suppl):S19-33.
- Hauschild VD, Schuh-Renner A, Lee T, Richardson MD, Hauret K, Jones BH. Using causal energy categories to report the distribution of injuries in an active population: An approach used by the U.S. Army. J Sci Med Sport. 2019;22(9):997-1003.
- Army Public Health Center. Survey of Injuries and Injury Risk Factors in the 2nd Brigade Combat Team, 3rd Infantry Division, Nov. 2014-Jan. 2015, Technical Report S.0030637-17. Accessed 15 March 2019. https://apps.dtic.mil/docs/citations/AD1036189
- Hauschild VD, Schuh A, Taylor BJ, et al. Identification of specific activities associated with fall-related injuries, active component, U.S. Army, 2011. MSMR. 2016; 23(6):2–9.
- Smith GS, Dannenberg AL, Amoroso PJ. Hospitalization due to injuries in the military. Evaluation of current data and recommendations on their use for injury prevention. Am J Prev Med. 2000;18(38):41-53.
- Bonnie RJ, Fulco CE, Liverman CT, eds. Reducing the Burden of Injury: Advancing Prevention and Treatment. Washington, D.C.: The National Academies Press; 1999.
- Currie G, Kerfoot KD, Donaldson C, et al. Are cost of injury studies useful? Inj Prev. 2000;6(3):175-176.
- Rice, DP, Hodgson TA, Kopstein AN. The economic costs of illness: a replication and update. Health Care Finance Rev. 1985;7(1):61-80.
- Changik J. Cost-of-illness studies: concepts, scopes, and methods. Clin Mol Hepatol. 2014;20(4):327-337.
- ICD-10 Framework: Injury Mortality Diagnosis Matrix. Centers for Disease Control and Prevention (CDC) website. Accessed 8 March 2019. https://www.cdc.gov/nchs/injury/ice/injury_matrix10.htm
- Defense Finance and Accounting Services (DFAS). Military Pay Charts 2017. Accessed 8 March 2019. https://www.dfas.mil/Portals/98/2017MilitaryPayChart.pdf
- Hauret KG, Taylor BJ, Clemmons NS, et al. Frequency and causes of non battle injuries air evacuated from Operations Iraqi Freedom and Enduring Freedom, U.S. Army, 2001-2006. Am J Prev Med. 2010;38(1 Suppl):S94-107.
- Army Public Health Center. The Cost of Army Injuries, Phase 1: Lower extremity fractures among active duty soldiers CY2017, Public Health Information Paper (PHIP) No. 12-04-1219. 2020. Army Public Health Center, Aberdeen Proving Ground, MD.