What are the new findings?
In the last decade, the most common vector-borne diseases among U.S. Armed Forces tended to be Lyme disease, malaria, Rocky Mountain spotted fever, dengue, and leishmaniasis. During 2014–2016, the pandemics of chikungunya and Zika virus transiently inserted those diseases into the top 5. The declining incidences of malaria and leishmaniasis during 2016–2020 are likely due to reduced numbers of service members assigned to endemic regions of the world.
What is the impact on readiness and force health protection?
The current findings reemphasize that the threat to service members from vector-borne diseases will vary according to the prevalent endemic diseases of specific geographic locations, the availability of protective vaccines, and the implementation of individual and group preventive measures.
Abstract
This report summarizes data from electronic reports of reportable medical events (RMEs) to examine the incidence of vector-borne infectious diseases among members of the U.S. Armed Forces during a recent 5-year period. Case reports of such diseases were characterized as confirmed, probable, or suspected by the senders of the RME reports. Records of inpatient and outpatient care were not searched to find additional cases. Lyme disease and malaria were the most common diagnoses among confirmed cases. The next most common diagnoses were Zika virus infection, Rocky Mountain spotted fever, and dengue. Those 5 diseases were responsible for 94% of all confirmed vector-borne diseases reported as RMEs. Among the 1,068 RMEs for vector-borne diseases (confirmed, probable, and suspected), there were only 105 such cases that could be linked to a record of hospitalization for the same diagnosis.
Background
The U.S. Armed Forces and the Department of Defense (DOD) have traditionally dedicated considerable effort to the prevention and treatment of vector-borne diseases that may adversely affect the ability of military service members to train for and execute their operational mission. A continuing element of that effort has been the performance of surveillance of vector-borne illnesses to guide preventive actions. The pages of the MSMR reflect over 25 years of surveillance studies to inform military leaders and preventive medicine/public health assets about the incidence of vector-borne diseases and appropriate steps to counter the associated threat. The February 2018 issue of the MSMR contained the results of the most recent, broad surveillance study of the most concerning vector-borne diseases.1 This article presents an updated review of this subject, utilizing a modified methodology for capturing the occurrence of cases.
Methods
The surveillance period was 1 Jan. 2016 through 31 Dec. 2020. The surveillance population included all active and reserve component service members in the Army, Navy, Air Force, or Marine Corps who served at any time during the surveillance period. It is DOD policy that cases of certain specified medical conditions and events of public health importance shall be reported electronically through military health channels for surveillance purposes.2 Conditions covered by this policy are referred to as reportable medical events (RMEs). The content of such electronic reports is stored in the databases of the Defense Medical Surveillance System (DMSS), which was used to ascertain cases for this analysis. The vector-borne diseases that are the focus of this report are listed in Table 1. Almost all vector-borne diseases of concern for military service members are designated as RMEs.
For this analysis, a "confirmed", "probable", or :"suspected" case was defined as an individual identified through an RME report of a vector-borne disease that was described as "confirmed", "probable" or "suspect" by having met specified laboratory or epidemiologic criteria.2 An individual could be counted once per lifetime for each type of vector-borne disease. For example, an individual could be counted once for malaria and once for leishmaniasis during the surveillance period. Individuals diagnosed as a case prior to the start of the surveillance period were excluded. Confirmed cases were prioritized over probable and suspected cases, respectively.
A case was considered to be hospitalized if they had an inpatient admission within 30 days before or after the date of onset reported in the RME. In addition, the inpatient record had to include a diagnosis for the vector-borne disease as listed in Table 1 in any of the diagnostic positions. The total number of cases hospitalized, as well as the percentage hospitalized and number of bed days were summarized for each vector-borne disease.
Results
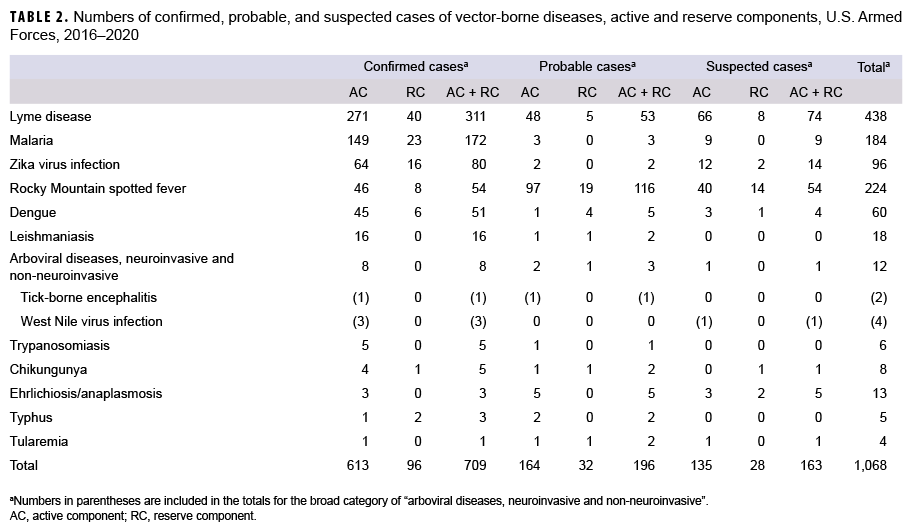
During the 5-year surveillance period, the electronic records of RMEs identified 709 confirmed cases of vector-borne diseases, 196 probable cases, and 163 suspected cases among service members of the active and reserve components (Table 2). Active component service members comprised 86% of confirmed cases, 84% of probable cases, and 83% of suspected cases. There were no RMEs for any of the diagnoses of hemorrhagic fevers, filariasis, plague, relapsing fever, or yellow fever. The category "Arboviral diseases, neuro-invasive and non-neuroinvasive" included 3 cases of confirmed West Nile virus infection, 1 case of confirmed tick born encephalitis (TBE), and 4 unspecified types, for a total of 8 confirmed cases in that category. Only the 14 diagnostic categories displayed in Table 2 had any RMEs during the 5-year period.
Of the total of 709 confirmed cases, 668 (94%) were associated with RME diagnoses of Lyme disease (n=311), malaria (n=172), Zika virus infection (n=80), Rocky Mountain spotted fever (RMSF) (n=54), and dengue fever (n=51). The other diagnoses that were reported as confirmed cases were much less commonly documented (Table 2).
The distribution of diagnoses among probable RME cases was different from that of confirmed cases. It was noteworthy that Lyme disease was the diagnosis for 53 (27%) of the 196 probable cases, but RMSF accounted for 116 (59%) of the total probable cases. None of the other diagnoses was reported more than 5 times as probable cases during the 5 year surveillance period (Table 2).
Among the suspected cases, the most common RMEs were for Lyme disease (n=74), RMSF (n=54), and Zika virus infection (n=14). Together those three diagnoses were the subject of 87% of suspected cases of RMEs (Table 2). For the results described below, the emphasis will be on confirmed cases.
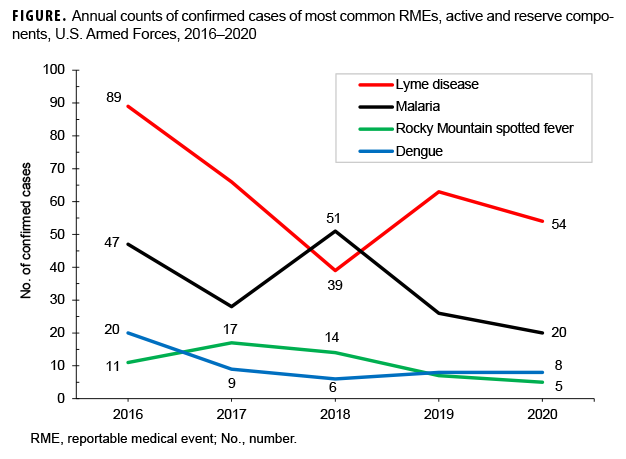
Lyme disease
Lyme disease accounted for 43.8% of all confirmed RME cases and was the most common of the vector-borne diseases reported during 2016–2020. The annual numbers of confirmed cases were greatest in 2016 and lowest in 2018, when the number of Lyme disease cases was actually lower than the count of malaria cases (Figure 1). The numbers of probable and suspected cases of Lyme disease (n=127) were actually lower than the counts for RMSF (n=170) during the surveillance period (Table 2).
Malaria
Diagnoses of malaria (n=172) contributed 24.2% of all confirmed RME cases of vector-borne diseases during the 5 year surveillance period. The highest count was in 2018 (n=51) but the most recent two years had the lowest counts of the period (n=26 and 20, respectively) (Figure 1). There were only 12 cases of malaria in RME reports of probable and suspected cases (Table 2).
Zika virus infection
Confirmed cases of Zika virus infection numbered 80 during the period (Table 2). However, 73 of those cases were reported in 2016, with the remainder reported in 2017 (n=4), 2019 (n=2), and 2020 (n=1) (data not shown). Zika virus was introduced into the Americas in 2015 and the case counts in the U.S. as well as in the U.S. Armed Forces peaked in 2016.3 Of the 16 service member cases reported as probable or suspected, 12 were reported in 2016 (data not shown).
Rocky Mountain spotted fever
Confirmed cases of RMSF (n=54), unlike all other diagnoses that are reportable, were outnumbered by reports of probable (n=116) and suspected (n=54) cases of RMSF (Table 2). This phenomenon is likely the result of the necessity to confirm the diagnosis of RMSF (and related rickettsial diseases) via the performance of acute and convalescent serological studies or other more sophisticated tests such as a PCR test for DNA, immunohistochemistry of a biopsy specimen, or a positive culture. The current RME guidelines include RMSF in the broader category of Spotted Fever Rickettsiosis, which includes conditions with similar clinical presentations that may be distinguished only with the testing procedures mentioned above.
Dengue
Of the total of 60 cases of dengue reported via RME, 51 were described as confirmed (Table 2). At least 18 of those confirmed cases were reported by an overseas treatment facility and an additional 14 cases were linked to an overseas travel location. The most commonly cited of those locations were Djibouti (n=7) and the Philippines (n=5). There were relatively few RME cases of dengue that were classified as probable (n=5) or suspected (n=4) (data not shown).
Leishmaniasis
There were 16 confirmed cases of leishmaniasis reported during the period but only 2 of them were reported in 2019 and none in 2020 (Table 2, data not shown). Of the 6 cases for which the reports mention a location where the service member may have acquired the infection, 5 specify either Iraq, Afghanistan, or Syria and 1 mentions Palau (data not shown). Probable cases numbered 2 and there were no suspected cases.
Arboviral diseases, neuroinvasive and nonneuroinvasive
The 3 confirmed cases and 1 suspected case of West Nile virus infection were diagnosed in the continental U.S. and the single confirmed and probable cases of tick-borne encephalitis were diagnosed in Germany (data not shown). Among the total of 12 cases that were reported in this broad category, 7 were associated with Germany and 5 with the U.S. (data not shown).
Other
The remaining 5 diagnostic categories of RMEs were associated with a total of 17 confirmed cases, 12 probable cases, and 7 suspected cases over the 5-year surveillance period (Table 2). The most recent confirmed cases of chikungunya were 2 that were diagnosed in 2019 and they were associated with recent travel to the Philippines and Djibouti, respectively (data not shown).
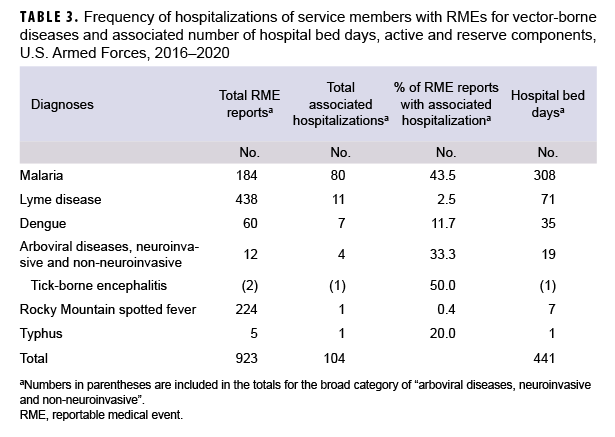
Hospitalizations
During the 5-year surveillance period, there were 1,068 RME reports submitted for confirmed, probable, and suspected cases. Associated with the service members who were the subjects of those reports, there were 105 instances of hospitalization for which the records of inpatient care specified the diagnosis of the reportable condition. Such hospitalizations reflected only 6 different reportable diagnoses (Table 3). Of the 184 reported cases of malaria, 43.5% were associated with hospitalizations (n=80) for which a malaria diagnosis was recorded. For Lyme disease, the 11 hospitalizations represented 2.5% of all RME diagnoses of that condition; for dengue, the 7 hospitalizations were associated with 11.7% of all RME diagnoses; for arboviral diseases, there were 4 hospitalizations representing 33.3% of all cases that were reported. Finally, there were single hospitalizations for RMSF and typhus that represented .4% and 20% of RMEs for those respective diagnoses (Table 3).
Editorial Comments
The identities of the most common vector-borne diseases in this analysis were similar to those documented in previous studies. For example, MSMR reports covering the years 1995–1999 and 2010–2016 noted that the most common diseases included Lyme disease, malaria, RMSF, dengue fever, and leishmaniasis, just as was the case for 2016–2020.1,4 The only exceptions to the lists of most common diseases were due to the pandemic occurrences of chikungunya and Zika virus infections starting in 2013.3,5
The methods employed in this surveillance study differed significantly from the two studies previously mentioned. The counts for 2016–2020 were based solely on RMEs electronically submitted by public health/preventive medicine specialists who evaluated the available information for each case in order to render an evaluation as to whether or not the diagnosis was confirmed, probable, or suspected. The previous studies utilized DMSS records of hospitalizations and/or outpatient encounters to identify cases. It is most noteworthy that using only the documentation of outpatient diagnoses to qualify as a "suspected" case, as was one of the criteria in 2010–2016, is a highly sensitive, but very non-specific means of identifying cases. The employment of just RMEs to identify and count cases of vector-borne diseases increases the probability they are true cases of the diseases of interest. However, the omission of inpatient and outpatient diagnoses of these diseases likely yields an underestimate of the true incidence of some of the conditions.
The analysis of hospitalizations among RME cases revealed that most reportable vector-borne diseases were not associated with a hospitalization within 30 days before or after the reported date of illness onset. The correlation between hospitalization and diagnosis of a reportable disease is mainly a reflection of the severity of illness. The diseases of interest in this study have a broad spectrum of clinical severity and, in particular, if a given disease can be readily treated with a highly effective antimicrobial agent, then rates of hospitalization may be quite low.
The reader is referred to the February 2018 MSMR article on this subject for further discussion of the topics of Lyme disease incidence in the U.S., the years of peak incidence of chikungunya and Zika virus infections, the declining incidence of leishmaniasis associated with reduced presence of service members in the Middle East, and the pitfalls of using outpatient diagnoses for surveillance.1
References
- O’Donnell FL, Stahlman S, Fan M. Surveillance for vector-borne diseases among active and reserve component service members, U.S. Armed Forces, 2010–2016. MSMR. 2018;25:8–15.
- Defense Health Agency. Armed Forces Reportable Medical Events. Guidelines and Case Definitions. January 2020.
- Ikejezie J, Shapiro CN, Kim J, et al. Zika virus transmission–Region of the Americas, May 15, 2015 – December 15, 2016. MMWR Morb Mortal Wkly Rep. 2017;66:329–334.
- Garvey AL. Five most common arthropodborne diseases among active duty service members in the U.S. Armed Forces, 1995-1999. MSMR. 2000;6:12–16.
- Fischer M, Staples JE. Notes from the field. Chikungunya virus spreads in the Americas – Caribbean and South America, 2013–2014. MMWR Morb Mortal Wkly Rep. 2014:63:500–501.