What Are the New Findings?
Among service members deployed during 2018, injury/poisoning, musculoskeletal diseases, and signs/symptoms accounted for more than half of the total health care burden while deployed. Compared to the distribution of major burden of disease categories documented in garrison, a relatively greater proportion of in-theater medical encounters due to respiratory infections, skin diseases, infectious/parasitic diseases, and digestive diseases was documented.
What Is the Impact on Readiness and Force Health Protection?
Injuries and musculoskeletal diseases account for a significant proportion of illness- and injury-related medical care in both deployed and non-deployed settings. However, while deployed, readiness may also be impacted by some infectious conditions associated with austere environmental and sanitary conditions.
Background
Every year, the MSMR estimates illness- and injury-related morbidity and health care burdens on the U.S. Armed Forces and the Military Health System (MHS) using electronic records of medical encounters from the Defense Medical Surveillance System (DMSS). These records document health care delivered in the fixed medical facilities of the MHS and in civilian medical facilities when care is paid for by the MHS. Health care encounters of deployed service members are documented in records that are maintained in the Theater Medical Data Store (TMDS), which is incorporated into the DMSS. Last year for the first time, TMDS morbidity burden analyses were included in the annual MSMR burden issue.1 This report examines the distributions of illnesses and injuries that accounted for medical encounters ("morbidity burdens") of active component members in deployed settings in the U.S. Central Command (CENTCOM) and the U.S. Africa Command (AFRICOM) areas of operations during the 2018 calendar year.
Methods
The surveillance population included all individuals who served in the active or reserve components of the U.S. Army, Navy, Air Force, or Marine Corps and who had records of health care encounters captured in the TMDS during the surveillance period. The analysis was restricted to encounters where the theater of care specified was CENTCOM or AFRICOM. By default, this excluded encounters in the U.S. Northern Command, U.S. European Command, U.S. Indo-Pacific Command, or U.S. Southern Command theater of operations. Encounters where the theater of operation was missing were included, as most of these were assumed to be from CENTCOM. TMDS-recorded medical encounters where the data source was identified as Shipboard Automated Medical System (e.g., SAMS, SAMS8, SAMS9) or where the military treatment facility descriptor indicated care was provided aboard a ship (e.g., USS George H.W. Bush or USS Dwight D. Eisenhower) were excluded from this analysis. Encounters from aeromedical staging facilities outside of CENTCOM or AFRICOM (e.g., the 779th Medical Group Aeromedical Staging Facility or the 86th Contingency Aeromedical Staging Facility) were also excluded. Inpatient and outpatient medical encounters were summarized according to the primary (first-listed) diagnoses (if reported with an International Classification of Diseases, 9th Revision, Clinical Modification [ICD-9-CM] code between 001 and 999 or beginning with V27 or with an International Classification of Diseases, 10th Revision, Clinical Modification [ICD-10-CM] code between A00 and T88 or beginning with Z37). Primary diagnoses that did not correspond to an ICD-9 or ICD-10 code (e.g., 1XXXX or 4XXXX) were not reported in this burden analysis.
In tandem with the methodology described on page 2 of this issue of the MSMR, all illness- and injury-specific diagnoses were grouped into 142 burden of disease-related conditions and 25 major categories based on a modified version of the classification system developed for the Global Burden of Disease (GBD) study.2 The morbidity burdens attributable to various conditions were estimated on the basis of the total number of medical encounters attributable to each condition (i.e., total hospitalizations and ambulatory visits for the condition with a limit of 1 encounter per individual per condition per day) and the numbers of service members affected by the conditions. In general, the GBD system groups diagnoses with common pathophysiologic or etiologic bases and/or significant international health policymaking importance. For this analysis, some diagnoses that are grouped into single categories in the GBD system (e.g., mental health disorders) were disaggregated. Also, injuries were categorized by the affected anatomic sites rather than by causes because external causes of injuries are not completely reported in TMDS records. It is important to note that because the TMDS has not fully transitioned to ICD-10 codes, ICD-9 codes appear in this analysis. In addition to the examination of the distribution of diagnoses by the 142 conditions and the 25 major categories of disease burden, a third analysis depicts the distribution of diagnoses according to the 17 traditional categories of the ICD system.
Results
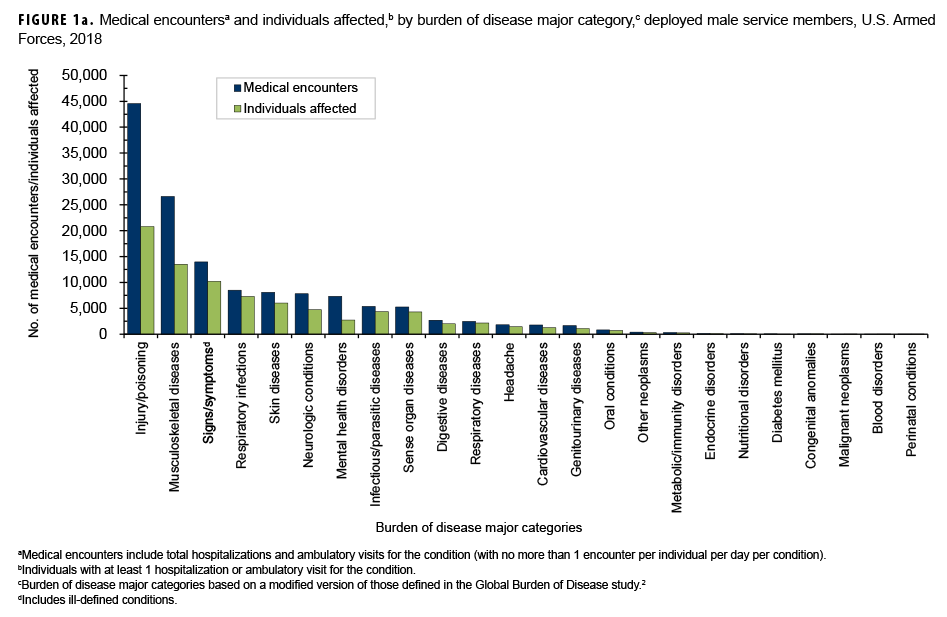
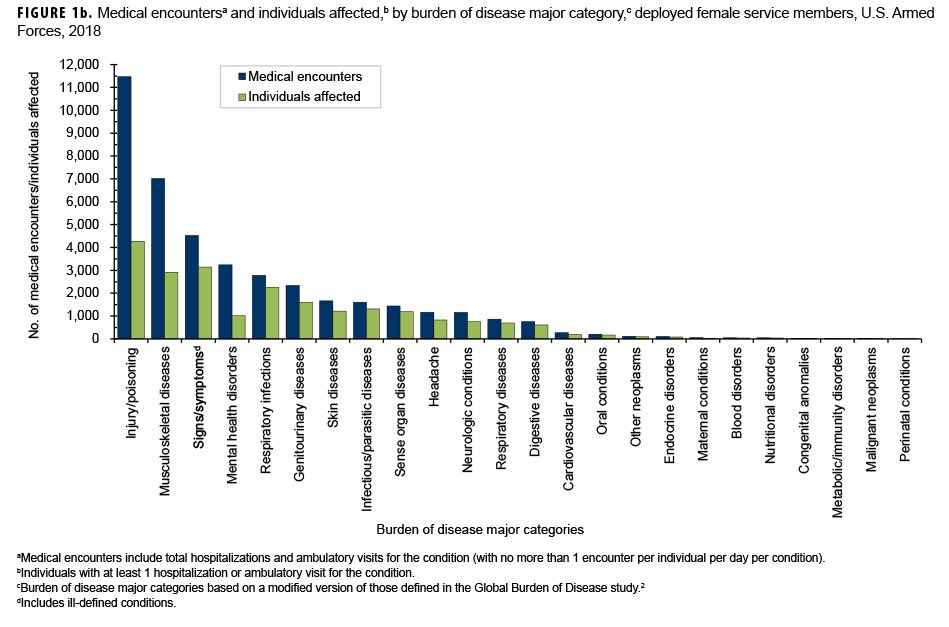
In 2018, a total of 180,940 medical encounters occurred among 66,627 individuals while deployed to Southwest Asia/Middle East and Africa. Of the total medical encounters, only 56 (0.03%) were indicated to be hospitalizations (data not shown). A majority of the medical encounters (77.4%), individuals affected (82.4%), and hospitalizations (89.3%) occurred among males (Figures 1a, 1b).
Medical Encounters/Individuals Affected by Burden of Disease Categories
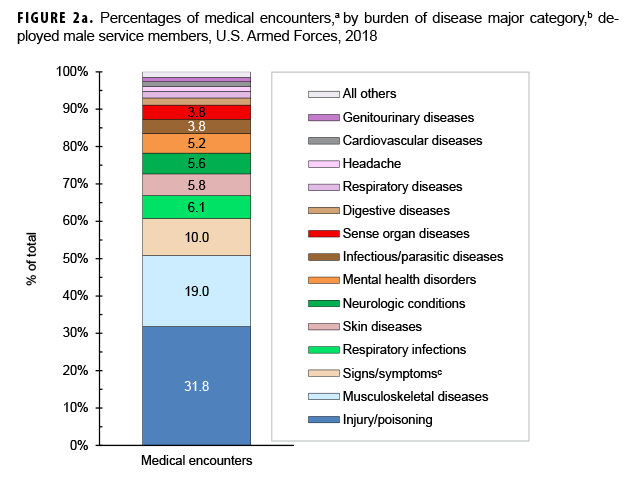
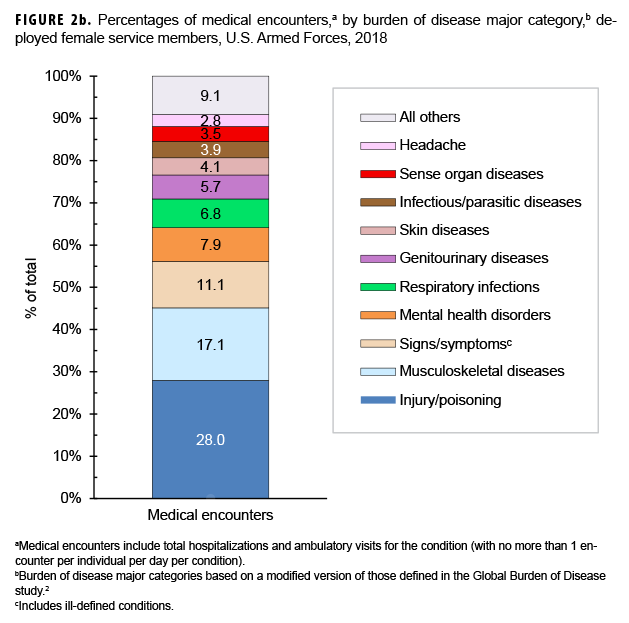
During 2018, the percentages of total medical encounters by burden of disease categories in deployed men and women were generally similar; in both sexes, more encounters were attributable to injury/poisoning, musculoskeletal diseases, and signs/symptoms (including ill-defined conditions) than any other categories (Figures 1a, 1b, 2a, 2b). Of note, females had a greater proportion of medical encounters for genitourinary diseases (5.7%) compared to males (1.2%). Females also had a slightly higher proportion of medical encounters for mental health disorders (7.9%) compared to males (5.2%).
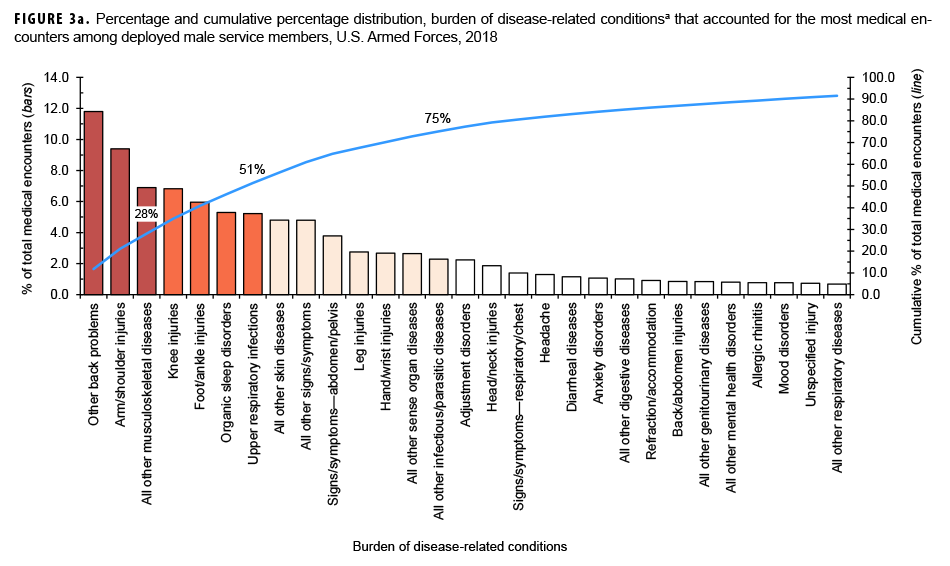
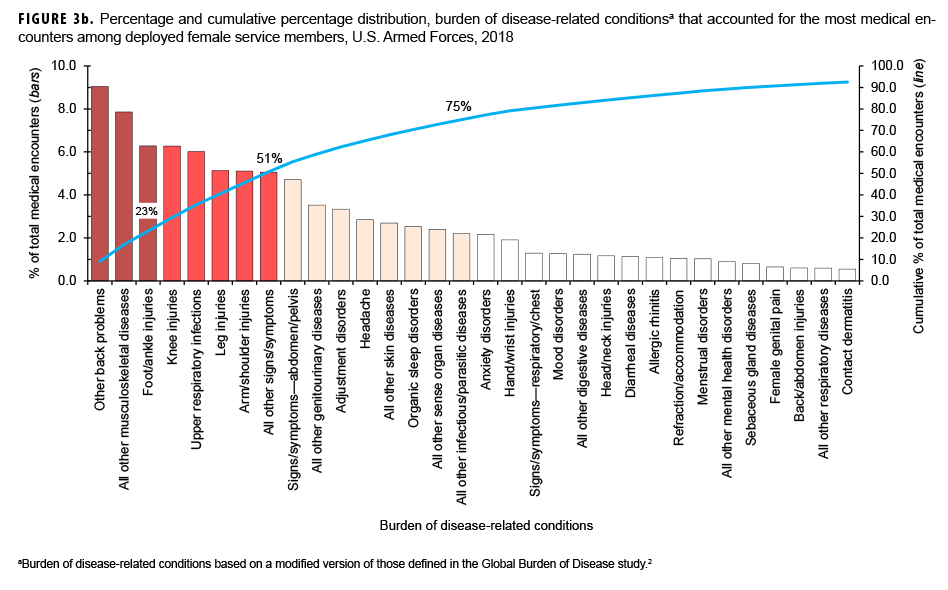
Among both males and females, 4 burden conditions (other back problems, all other musculoskeletal diseases, knee injuries, and foot and ankle injuries) were among the top 5 burden conditions that accounted for the most medical encounters in 2018 (Figures 3a, 3b). The remaining burden conditions among males and females were arm and shoulder injuries and upper respiratory infections, respectively.
The 4-digit ICD-10 code with the most medical encounters in the other back problems category during 2018 was lumbago/low back pain (data not shown). Among both men and women, for all other musculoskeletal diseases, the most common 4-digit ICD codes were for pain in limb and cervicalgia. The most common 4-digit ICD-10 code for arm and shoulder injuries among males and for foot and ankle injuries among females was for pain in joint (data not shown).
Of note, among males, less than 0.3% of all medical encounters during deployment were associated with any of the following major morbidity categories: metabolic/immunity disorders, endocrine disorders, nutritional disorders, diabetes mellitus, congenital anomalies, malignant neoplasms, blood disorders, and perinatal conditions (Figure 1a). Among females, less than 0.3% of all medical encounters during deployment were associated with maternal conditions, blood disorders, nutritional disorders, congenital anomalies, metabolic/immunity disorders, malignant neoplasms, diabetes mellitus, and perinatal conditions (Figure 1b).
Among both sexes in 2018, injury/poisoning, musculoskeletal diseases, and signs/symptoms were the top 3 categories that affected the most individuals; musculoskeletal diseases ranked second among males and third among females (Figures 1a, 1b).
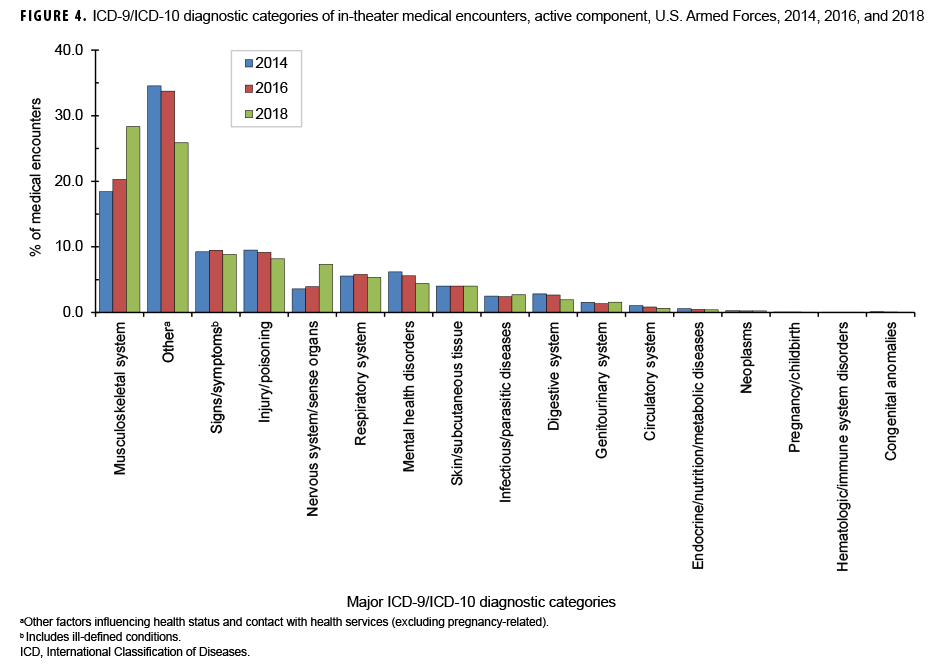
Medical Encounters by Major ICD-9/ICD-10 Diagnostic Category
In 2018, among the 17 major ICD-9/ICD-10 diagnostic categories, the largest percentages of medical encounters were attributable to musculoskeletal system and "other" (includes factors influencing health status and contact with health services as well as external causes of morbidity) (Figure 4). The percentage of medical encounters attributable to musculoskeletal system conditions increased from 2014 through 2018 and the percentage attributable to "other" decreased during the same period. Of note, the percentages of medical encounters attributable to injury/poisoning and mental health disorders decreased slightly from 9.5% in 2014 to 8.2% in 2018 for injury/poisoning and from 6.2% to 4.4% for mental health disorders. However, the percentage of medical encounters attributable to disorders of the nervous system and sense organs doubled from 3.6% in 2014 to 7.3% in 2018. The percentages of medical encounters attributable to other major ICD-9/ICD-10 diagnostic categories were relatively similar during the years 2014, 2016, and 2018.
Editorial Comment
This report documents the morbidity and health care burden among U.S. military members while deployed to Southwest Asia/Middle East and Africa during 2018. Similar to results from earlier surveillance periods,1,3 3 burden categories—injury/poisoning, musculoskeletal diseases, and signs/symptoms—together accounted for 50% or more of the total health care burden among both male and female deployers. However, the 2018 percentages of encounters due to mental health disorders among males and females (5.2% and 7.9%, respectively) were much smaller than the corresponding percentages during 2008–2014 (13.1% and 13.8%, respectively).3
Compared to the distribution of major burden of disease categories documented in garrison, this report demonstrates a relatively greater proportion of in-theater medical encounters due to respiratory infections, skin diseases, infectious and parasitic diseases, and digestive diseases.4 The lack of certain amenities and greater exposure to austere environmental conditions may have compromised hygienic practices and contributed to this finding. However, 4 of the top 5 major burden of disease categories in-theater—injury/poisoning, musculoskeletal diseases, signs/symptoms, and mental health disorders—were the same as those reported in non-deployed settings.4 Injury and musculoskeletal diseases ranked first and second, respectively, in both settings. In garrison settings, mental health disorders, signs/symptoms, and neurologic conditions ranked third through fifth.4 In contrast, sign/symptoms, respiratory infections, and mental health disorders ranked third through fifth in deployed settings. The similarity in these top conditions is likely attributable to the fact that both deployed and non-deployed populations generally comprise young and healthy individuals undergoing strenuous physical and mental tasks. Some of the similarity in the top conditions could also be attributed to service members receiving follow-up care once out of theater. For example, a service member medically evacuated out of theater for an injury could have encounters for injury recorded in both deployed and non-deployed (hospital or ambulatory care) settings.
Encounters for certain conditions are not expected to occur often in deployment settings. For example, the presence of some conditions (e.g., diabetes mellitus, pregnancy, or congenital anomalies) makes the affected service members ineligible for deployment. As a result of this selection process, deployed service members are generally healthier than their non-deployed counterparts and, specifically, less likely to require medical care for conditions that preclude deployment. The overall result of such predeployment medical screening is diminished health care burdens (as documented in the TMDS) related to certain disease categories.
Interpretation of the data in this report should be done with consideration of some limitations. Not all medical encounters in theaters of operation are captured in the TMDS. Some care is rendered by medical personnel at small, remote, or austere forward locations where electronic documentation of diagnoses and treatment is not feasible. As a result, the data described in this report likely underestimate the total burden of health care actually provided in the areas of operation examined. In particular, some emergency medical care provided to stabilize combat-injured service members before evacuation may not be routinely captured in the TMDS. Another limitation derives from the potential for misclassification of diagnoses due to errors in the coding of diagnoses entered into the electronic health record. Although the aggregated distributions of illnesses and injuries found in this study are compatible with expectations derived from other examinations of morbidity in military populations (both deployed and non-deployed), instances of incorrect diagnostic codes (e.g., coding a spinal cord injury using a code that denotes the injury was suffered as a birth trauma rather than using a code indicating injury in an adult) warrant care in the interpretation of some findings. Although such coding errors are not common, their presence serves as a reminder of the extent to which this study depends on the capture of accurate information in the sometimes austere deployment environment in which health care encounters occur.
References
- Armed Forces Health Surveillance Branch. Morbidity burdens attributable to various illnesses and injuries, deployed active and reserve component service members, U.S. Armed Forces, 2017. MSMR. 2018;25(5):26–31.
- Murray CJ and Lopez AD, eds. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Cambridge, MA: Harvard University Press; 1996:120–122.
- Armed Forces Health Surveillance Branch. Morbidity burdens attributable to various illnesses and injuries in deployed (per Theater Medical Data Store [TMDS]) active and reserve component service members, U.S. Armed Forces, 2008–2014. MSMR. 2015;22(8):17–22.
- Armed Forces Health Surveillance Branch. Absolute and relative morbidity burdens attributable to various illnesses and injuries, active component, U.S. Armed Forces, 2018. MSMR. 2019;26(5):2–9.