Abstract
During 2000–2017, a total of 170,878 active component service members underwent a first-occurring vasectomy, for a crude overall incidence rate of 8.6 cases per 1,000 person-years (p-yrs). Among the men who underwent incident vasectomy, 2.2% had another vasectomy performed during the surveillance period. Compared to their respective counterparts, the overall rates of vasectomy were highest among service men aged 30–39 years, non-Hispanic whites, married men, and those in pilot/air crew occupations. Male Air Force members had the highest overall incidence of vasectomy and men in the Marine Corps, the lowest. Crude annual vasectomy rates among service men increased slightly between 2000 and 2017. The largest increases in rates over the 18-year period occurred among service men aged 35–49 years and among men working as pilots/air crew. Among those who underwent vasectomy, 1.8% also had at least 1 vasectomy reversal during the surveillance period. The likelihood of vasectomy reversal decreased with advancing age. Non-Hispanic black and Hispanic service men were more likely than those of other race/ethnicity groups to undergo vasectomy reversals.
What Are the New Findings?
During 2000–2017, 170,878 service men underwent vasectomies (rate: 8.6 cases per 1,000 p-yrs). Annual rates increased 34% during the period. Rates were highest among men who were aged 30–39 years, non-Hispanic white, married, or in the Air Force. A total of 3,134 (1.8%) men underwent vasectomy reversal procedures. Younger men were more likely to seek reversals.
What Is the Impact on Readiness and Force Health Protection?
Vasectomy is a safe, simple, economical, and effective method of permanent contraception. Usually performed on an outpatient basis, vasectomies have a minimal impact on readiness. Service mens' choice of vasectomy should be decided with medical personnel who can provide counsel about the factors important in deciding on permanent sterilization, such as age, number of children, and long term impact.
Background
In the U.S., vasectomy is performed less often than female sterilization despite it being a safer, simpler, more economical, and equally effective option for permanent contraception.1 U.S. data from the 2006–2010 National Survey for Family Growth (NSFG) estimated that 6.6% of men aged 15–44 years reported having had a vasectomy; this proportion increased with age, reaching up to 16% among men aged 36–45 years.2 This prevalence estimate is relatively unchanged from the 2002 NSFG estimate of 6.2%.3,4 However, these survey-based estimates are limited by a low response rate and sample size.4,5 Results of U.S. studies using claims data show that the prevalence of vasectomies decreased from 2007 through 2015 among men aged 18–64 years with employer-based insurance, and prevalence estimates decreased across all age groups and in all locations of the country.5,6 The incidence of vasectomy in the U.S. is poorly characterized. However, 1 retrospective survey-based study conducted in 2002 using a random sample of urologists, family physicians, and general surgeons from the American Medical Association Physician Masterfile yielded an annual vasectomy incidence rate of approximately 10 per 1,000 men aged 25–49 years.7
The vasectomy procedure involves isolation and interruption or occlusion of each vas deferens (vas) and is most typically performed in an outpatient setting.5 The 2 most common surgical techniques for accessing/isolating the vas during vasectomy are the conventional method and minimally invasive techniques (including the no-scalpel vasectomy technique).8 The conventional vasectomy (CV) technique is an open-style procedure that involves the use of a scalpel to make 1 midline incision or bilateral incisions on the scrotum.9 Incisions are usually 1.5–3.0 cm in length, and no special instruments are used during CV.7,9 Minimally invasive vasectomy (MIV) techniques use a percutaneous entry into the scrotum employing a sharp, forceps-like instrument.9 MIV includes any vas isolation procedure that incorporates 2 key surgical principles—small (<10 mm) openings in the scrotal skin (either as a single midline opening or as bilateral openings) and minimal dissection of the vas and perivasal tissues using a vas ring clamp and vas dissector or similar special instruments.8 After isolation, the vas is cut, cauterized, tied, or occluded using clips or occlusive implants.9 In the U.S., nearly all vasectomy techniques use complete division of the vas with or without excision of a segment of the vas.7 The available evidence indicates that a minimally invasive vas isolation procedure results in a significantly lower risk of postoperative complications (e.g., bleeding, postoperative pain, or infection) than CV.10 In addition, there are no significant differences in the effectiveness (azoospermia or absence of motile sperm) of the 2 procedures.10 The most recent (2012) American Urological Association guideline proposed as a standard that isolation of the vas should be performed using an MIV technique.8
Vasectomy reversal prevalence and trends in the general U.S. population are not well described. Results of studies conducted during the past 25 years indicate that up to 6% of men who undergo surgical sterilization will seek vasectomy reversal later.11–13 Vasectomy reversal procedures include vasovasostomy and the more technically challenging vasoepididymostomy.14 Vasovasostomy involves the reconnection of segments of the vas above and below an obstruction.14 Vasoepididymostomy involves connection of the vas to the epididymis in order to bypass an epididymal obstruction.14 Limited data are available on vasectomy reversal procedure patterns in the U.S.15
There are few published studies of vasectomy and vasectomy reversal among the U.S. military population. One administrative data-based study described the incidence of vasectomy and the demographic characteristics of U.S. active duty male service members aged 18–50 years who received vasectomies during 2000–2009.16 This study searched the Career History Archival Medical and Personnel System database for all records with an ICD-9 diagnosis code for vasectomy. The overall incidence of vasectomy was 7.1 per 1,000 service men, with an age-adjusted overall rate of 8.7 per 1,000 service men.16 A subsequent study using the same data source focused on the correlates of vasectomy reversal among the same group of vasectomized military members.17 Among the service men who had vasectomies, approximately 5% underwent subsequent vasectomy reversal.17 However, the published incidence estimate from this study did not appear to include percutaneous ligation vasectomies.16,17 Moreover, the vasectomy reversal-focused study used only 1 Current Procedural Terminology (CPT) code to identify vasovasostomies; vasoepididymostomies were not included in the analysis. Neither study described the incidence of vasectomy by military characteristics.16,17
To address these gaps, the current analysis describes the overall and annual incidence rates of vasectomy among active component service men during 2000–2017 by demographic and military characteristics. In addition, the median age at incident vasectomy and the time between incident vasectomy and first vasectomy reversal are described.
Methods
The surveillance period was 1 Jan. 2000 through 31 Dec. 2017. The surveillance population included all men who served in the active component of the Army, Navy, Air Force, or Marine Corps at any time during the surveillance period. Diagnoses were ascertained from administrative records of all medical encounters of individuals who received care in fixed (i.e., not deployed or at sea) medical facilities of the Military Health System (MHS) or civilian facilities in the purchased care system documented in the Defense Medical Surveillance System (DMSS).
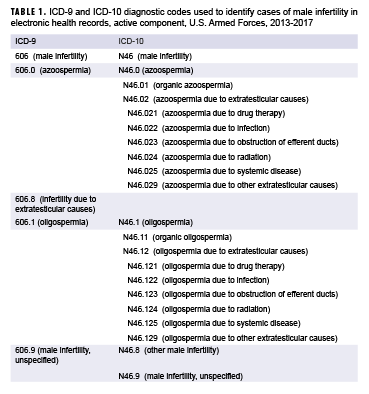
Vasectomies were defined by inpatient or outpatient medical encounters with a qualifying procedural code for the interruption/ligation of the vas coded in any position (Table 1). The incident date was the date of the first qualifying medical encounter. An individual was considered as having had an incident vasectomy once per lifetime. However, men could be counted as having a repeat vasectomy once per year in the years following their incident vasectomy. Men who had their first vasectomy prior to the start of the surveillance period were excluded from the analysis. If multiple encounters occurred on the same incident date, inpatient encounters were prioritized over outpatient. Incidence rates were calculated as incident vasectomies per 1,000 person-years (p-yrs). Median age at incident vasectomy was computed overall and by race/ethnicity group. The distribution of incident vasectomy counts by location (facility and installation name) also was examined. In addition, the number of incident vasectomy cases who underwent subsequent/repeat vasectomies during the surveillance period was computed.
Vasectomy reversals were identified among men who underwent an incident vasectomy during the surveillance period, and reversals were similarly defined by inpatient or outpatient medical encounters with a qualifying procedural code in any position (Table 2). Men could be counted as having repeated vasectomy reversals once per year in the years following their incident vasectomy. Vasectomy reversals were categorized as vasovasostomy (CPT code 55400; PR codes 63.81, 63.82, 63.84, 63.85, 63.89, 0VQJ*, 0VQK, 0VQL*, 0VQN*, 0VQP*, 0VQQ*, or OVPR*) or vasoepididymostomy (CPT codes 54900, 54901; PR codes 63.83, 0V1N*, 0V1P*, or 0V1Q*). The number of unique individuals who had 1 reversal and the number who had 2 or more reversals was determined from among the incident vasectomy cases who underwent vasectomy reversals. In addition, the time between incident vasectomy and first vasectomy reversal was examined by age group.
Results
Vasectomy
During 2000–2017, a total of 170,878 active component service members underwent a first-occurring vasectomy, for a crude overall incidence rate of 8.6 cases per 1,000 p-yrs (Table 3). The vast majority of these vasectomies were performed during outpatient encounters (n=170,601; 99.8%). More than four-fifths (n=145,721; 85.3%) of incident vasectomies took place in military treatment facilities (MTFs) compared with 14.7% in non-military medical facilities (outsourced care). Among the 170,878 men who underwent incident vasectomy, 3,729 (2.2%) had another vasectomy performed during the surveillance period. Of the men who underwent repeated vasectomies, 37 had more than 1 repeated vasectomy (data not shown).
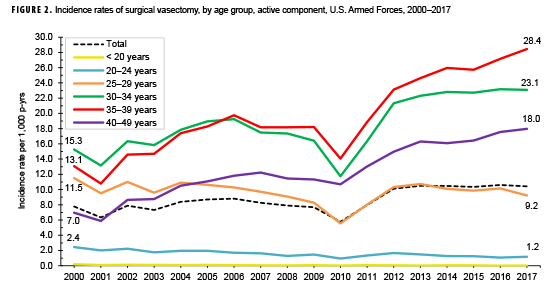
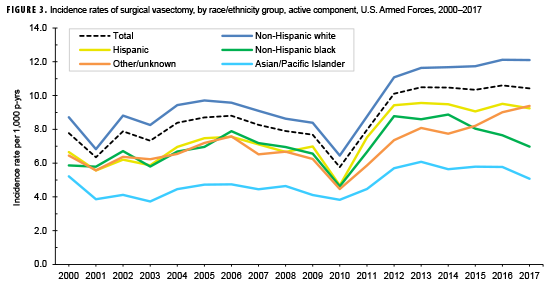
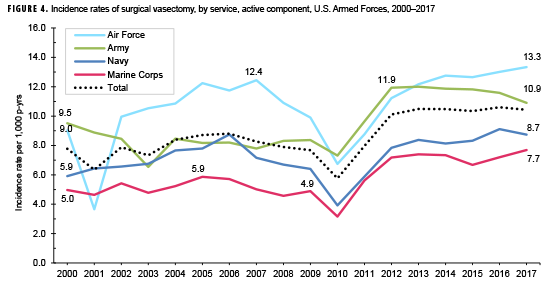
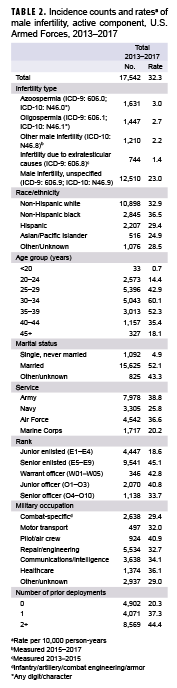
The crude overall incidence of vasectomy was highest among men aged 35–39 years (18.8 per 1,000 p-yrs) and those aged 30–34 years (18.4 per 1,000 p-yrs) (Table 3). The overall incidence was highest among non-Hispanic white service men (9.5 per 1,000 p-yrs) and lowest among Asian/Pacific Islanders (4.8 per 1,000 p-yrs). Overall rates were similar among Hispanic service men (7.7 per 1,000 p-yrs), those with other/unknown race/ethnicities (7.0 per 1,000 p-yrs), and non-Hispanic black service men (7.0 per 1,000 p-yrs). Married service men had the highest overall incidence of vasectomy (15.1 per 1,000 p-yrs) relative to men with other or unknown marital statuses (7.1 per 1,000 p-yrs) and those who were single and never married (0.5 per 1,000 p-yrs) (Table 3). Compared with their respective counterparts, men serving in the Air Force had the highest overall incidence of vasectomy (10.6 per 1,000 p-yrs) and men in the Marine Corps had the lowest (5.7 per 1,000 p-yrs). Among the different ranks, incidence of vasectomy was highest among senior officers (18.5 per 1,000 p-yrs) and lowest among junior enlisted service men (2.3 per 1,000 p-yrs). Across military occupations, overall incidence rates of vasectomy were highest among service men in pilot/air crew occupations (15.0 per 1,000 p-yrs) and lowest among those working in motor transport (6.6 per 1,000 p-yrs) or other/unknown (6.9 per 1,000 p-yrs) occupations.
The median age at incident vasectomy was 32 years (interquartile range [IQR]=29–37) (data not shown). Crude comparisons of age at incident vasectomy by race/ethnicity group showed that Hispanic service men had the youngest median age at vasectomy (median=31 years; IQR=28–36), while Asian/Pacific Islander service men had the oldest median age at vasectomy (median=35 years; IQR=30–39). Median age at incident vasectomy was similar among service men who were non-Hispanic white (median=32 years; IQR=29–37), non-Hispanic black (median=33 years, IQR=29–37), or of other/unknown race/ethnicity (median=32 years; IQR=29–36) (data not shown).
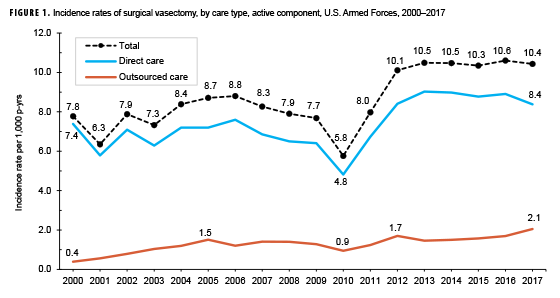
Over the course of the surveillance period, annual incidence rates of vasectomy increased slightly from 7.8 cases per 1,000 p-yrs in 2000 to 10.4 cases per 1,000 p-yrs in 2017 (34.2% increase). During the first 10 years of the period, crude annual incidence rates of vasectomy fluctuated between 6.3 and 8.8 per 1,000 p-yrs (Figure 1). Annual rates of vasectomy reached their lowest point in 2010 at 5.8 per 1,000 p-yrs, after which rates increased to 10.1 per 1,000 p-yrs in 2012. After 2012, annual rates of vasectomy leveled off and remained between 10.3 and 10.6 per 1,000 p-yrs through the end of the surveillance period. In 2017, the annual rate of incident vasectomy performed in non-military facilities (2.1 per 1,000 p-yrs) was more than 5 times the rate in 2000 (0.4 per 1,000 p-yrs) (Figure 1). By age group, the largest increases over the 18-year period were seen among service men aged 35–39 years (117.8%) and among those aged 40–49 years (158.4%). Among service men in the youngest age group (<20 years), annual vasectomy rates were low and relatively stable (Figure 2).
Throughout the surveillance period, annual rates of vasectomy among non-Hispanic white service men were consistently higher than rates among service men in the other race/ethnicity groups (Figure 3). From 2012 through 2017, annual vasectomy rates plateaued among Hispanic and Asian/Pacific Islander service men, with rates among non-Hispanic white service men and those of other/unknown race/ethnicity increasing slightly. Annual rates among non-Hispanic black service men decreased slightly between 2014 and 2017. During the surveillance period, annual rates of vasectomy increased slightly in each service (Figure 4). Between 2002 and 2009, annual vasectomy rates were markedly higher among men in the Air Force than among men in the other services. During the surveillance period, annual rates of vasectomy increased slightly among service men in all military occupations except those working as pilot/air crew; pilot/air crew rates increased 140.7% over the course of the 18-year period (9.2 per 1,000 p-yrs in 2000 and 22.2 per 1,000 p-yrs in 2017) (data not shown).
During the surveillance period, the largest number of incident vasectomies was performed at Naval Medical Center (NMC) Portsmouth, VA (n=7,726) (Table 4). This was followed by NMC San Diego, CA (n=5,905), Fort Bragg, NC (n=5,900), and Fort Hood, TX (n=5,613). The locations outside of the U.S. with the largest number of incident vasectomies performed included Landstuhl, Germany (n=3,271), Okinawa, Japan (n=1,862), Seoul, South Korea (n=1,548), and Lakenheath, England (n=1,439) (data not shown).
Vasectomy reversal
Among the 170,878 service men who underwent incident vasectomy, a total of 3,134 (1.8%) also had at least 1 vasectomy reversal during the surveillance period (Table 5). Among these, 83 (2.6%) men had more than 1 vasectomy reversal (data not shown). Vasectomy reversal was more common among men who had vasectomy performed during an inpatient stay (4.0%) compared with an outpatient encounter (1.8%). Among those who had their vasectomies performed at an MTF, 1.9% had a vasectomy reversal compared with 1.3% who had their vasectomy at an outsourced care facility (Table 5).
During 2000–2017, the most common type of vasectomy reversal performed among active component service members was vasovasostomy (95.3% of total medical encounters for reversals; 95.2% of the total number of men affected) (data not shown). A total of 3,006 service men had at least 1 vasovasostomy performed during the surveillance period, and 150 service men had at least 1 vasoepididymostomy performed during the surveillance period. A total of 80 service men had 2 vasectomy reversals, and 3 had 3 reversals (data not shown). Of the 3,134 men who underwent vasectomy and subsequent vasectomy reversal during the surveillance period, nearly two-fifths (39.0%) had the reversal 6 or more years after the initial vasectomy and approximately one-quarter (25.1%) underwent vasectomy reversal 2–3 years after the initial vasectomy. A similar proportion (24.9%) of the men who underwent vasectomy reversal underwent the procedure 4–5 years after the initial vasectomy. Slightly more than one-tenth (11.1%) of the men who underwent vasectomy reversal did so less than 2 years after the initial vasectomy (data not shown).
The likelihood of vasectomy reversal decreased with advancing age (Table 5). Almost 5% of the service men who were less than 20 years of age at the time of incident vasectomy later underwent vasectomy reversal. A similar proportion (5.0%) of the service men aged 20–24 years at the time of vasectomy went on to receive vasectomy reversals compared with 3.1% of service members aged 25–29 years, 1.7% aged 30–34 years, 0.7% aged 35–39 years, and 0.4% aged 40–49 years. None of the service men who were 50 years of age or older at the time of vasectomy had documentation of a vasectomy reversal during the surveillance period. Non-Hispanic black (2.3%) and Hispanic (2.3%) service men were more likely than those of other/unknown race/ethnicity (2.0%), non-Hispanic whites (1.7%), or Asian/Pacific Islanders (1.5%) to receive vasectomy reversals. In addition, vasectomy reversals were more likely to be performed among service men who had undergone vasectomy while single, never married (2.6%) or of other/unknown marital status (2.6%) compared with service men who had vasectomies while they were married (1.8%). Among the services, vasectomized men in the Army (2.4%) were more likely to have vasectomy reversals compared with men in the Air Force (1.5%), Navy (1.4%), or Marine Corps (1.3%). Those who had vasectomies performed while they were junior enlisted rank (3.1%) were more likely to later undergo vasectomy reversal than service men in any other rank category, including junior officers (1.8%). Service men who were working as pilots/air crew at the time of vasectomy (0.9%) were less likely to undergo vasectomy reversal than vasectomized service men in any other occupational category.
Editorial Comment
The results of the current study show that the crude annual incidence rates of vasectomy among active component service members increased slightly between 2000 and 2017. Data on trends in incidence of vasectomy in the general U.S. population during a comparable time period were not available at the time of this report, precluding comparisons to the current results. U.S. studies using claims data have shown that the prevalence of vasectomies decreased from 2007 through 2015 among men with employer-based insurance in all age groups.5,6 However, the generalizability of these claims-based findings is limited by the lack of inclusion of self-insured, Medicaid, or uninsured patients.5,6
The crude overall vasectomy incidence rate of 8.6 per 1,000 p-yrs observed in the current study is very similar to the age-adjusted rate of 8.7 per 1,000 service men reported by Santomauro et al. in their study of active duty service men but slightly lower than that for the U.S. general population (10 per 1,000 men aged 25–49).7,16 As noted by Santomauro and colleagues, this finding suggests that U.S. active component service men's access to no-cost care through the MHS is not associated with more vasectomies than in the general population.16 There are no formal U.S. Department of Defense policies regarding vasectomies for active component service members. However, there are clinically recognized standards for consideration of a sterilization procedure for a service man, including age, number of children, and reasons for desiring the procedure. While the determination of whether a patient is a good candidate for vasectomy is dependent on the critical judgement of the provider performing the procedure, the decision to pursue vasectomy is generally the product of joint decision making.
In the current study, the crude overall incidence of vasectomy was highest among service men aged 30–39 years, non-Hispanic white service men, and those who were married at the time of vasectomy. These demographic subgroup-specific findings mirror the results of vasectomy studies in the general U.S. population.2,4,18,19 Multiple studies have described the association between race and vasectomy utilization, with non-Hispanic white men being more likely to use vasectomy as a means of permanent contraception compared to men in other race/ethnicity groups.2,7,20,21 Santomauro et al.'s study of active duty service men also reported a higher vasectomy rate among non-Hispanic whites compared to non-Hispanic blacks; data on other race/ethnicity groups were not available for analysis.16 In the current study, Asian/Pacific Islander service men had the lowest overall vasectomy incidence rate. At the time of this report, only 1 U.S. study reported finding that Asians had the lowest rate of vasectomy relative to other race/ethnicity groups.20
The reasons underlying differences in vasectomy rates by race/ethnicity are likely multifactorial. Possible explanations include cultural differences in factors such as preferences for children, union stability, and differential contact with the health care system.7,21,22 However, even among continuously married couples, non-white/minority men are far less likely to undergo vasectomy than their white counterparts.22 The current finding that married status is positively associated with vasectomy occurrence is consistent with the results of several U.S. studies.2,18,23
The median age at incident vasectomy in the current study was 32 years. This finding is consistent with results from Santomauro et al. who reported a mean age at vasectomy of 32.6 years among active duty service men.16 In addition, the median age at vasectomy in the current study falls within the range of median and mean ages reported in the published literature from NSFG studies.2,4,18 U.S. administrative data-based studies report a median age at vasectomy of 38 years among employer-insured men.5,6 In the current analysis, Hispanic service men had the youngest median age at vasectomy and Asian/Pacific Islander service men had the oldest median age at vasectomy. In the U.S., it has been noted that Asian men have an older mean paternal age compared with the mean paternal ages of non-Hispanic whites and non-Hispanic blacks.24 This older paternal age among Asian men in the general U.S. population may explain, at least in part, the older age at vasectomy observed among Asian/Pacific Islander service men in the current study.
Results of the current analysis also showed that while more than four-fifths of incident vasectomies took place in MTFs during 2000–2017, the annual rate of incident vasectomy performed in non-military facilities increased more than 5-fold from the beginning to the end of the surveillance period.
The rate of repeat vasectomy observed in the current study was 2.2%. In the U.S., the risk of vasectomy failure requiring repeat vasectomy has been noted to be less than 1% provided that a technique for vas occlusion known to have a low occlusive failure rate was used.1,7,25,26 However, estimates of the rates of repeated vasectomy in the U.S. are derived from studies of vasectomy failure as measured by the number and timing of tests and the end points accepted and not from administrative data on the number of actual procedures performed.10 No U.S. estimates of the number of repeated vasectomy procedures were available at the time of this report.
During 2000–2017, 1.8% of the service men who had vasectomies also underwent vasectomy reversal during the surveillance period. This rate is lower than the approximately 6% vasectomy reversal rate reported for the general U.S. population.11–13 Vasectomy reversals are offered in the MHS but require general anesthesia and reserved time in the operating room. Vasectomy reversal is available to active component service members. However, TRICARE, the civilian care component of the MHS, does not cover the cost of vasectomy reversal unless medically necessary.27
The results of the current analysis corroborate findings of earlier studies, which showed that younger men were more likely to seek vasectomy reversal.12,17,28 Several potential reasons for this association have been posited, including a higher likelihood of divorce and remarriage (especially to a nulliparous partner), an altered attitude toward family size, and an improved financial situation as these younger men age.12,17,28–31 The current finding that vasectomy reversals were more likely to be performed among service men who underwent vasectomy while single may suggest that a change in marital status occurred after vasectomy.
In the current analysis, non-Hispanic black and Hispanic service men were more likely than those of other race/ethnicity groups to undergo vasectomy reversals; Asian/Pacific Islander service men were the least likely to have vasectomy reversals. In their study of active duty service men, Masterson et al. also reported that Asian service men were less likely than non-Hispanic white service men to undergo vasectomy reversal; Hispanics were not represented in their study because they were not identified in the data source.17
Results of the current study should be interpreted in the context of several important limitations. First, as incident vasectomies were identified based on the presence of a qualifying ICD-9 or ICD-10 inpatient procedural code or a qualifying outpatient CPT code recorded during a health care encounter, the validity of the results depends upon the accuracy of the physician-assigned procedural coding generated by a given encounter. In addition, it is possible that some of the vasectomies identified in the current analysis were performed for medical or therapeutic reasons (e.g., groin pain) and not for sterilization. Laparoscopic vasectomies were not included in the current analysis because there is no specific CPT code for this procedure. However, because this is the least commonly performed vas procedure, the number of missed cases is likely small.9 As with vasectomies, it is possible that some of the vasectomy reversals included in the current analysis were not carried out to restore fertility. While the vast majority of vasovasostomies are performed to reverse a prior vasectomy, the procedure is occasionally indicated for the repair of vas injury secondary to prior surgery or trauma.14 Finally, given the varying lengths of follow-up due to service members' departure from active service or the end of the study period, there were likely additional vasectomy reversals that were not captured in these data.
Another limitation of the current analysis is related to the implementation of MHS GENESIS, the new electronic health record for the MHS. For 2017, medical data from sites that were using MHS GENESIS are not available in DMSS. These sites include Naval Hospital Oak Harbor, Naval Hospital Bremerton, Air Force Medical Services Fairchild, and Madigan Army Medical Center. Therefore, medical encounter data for individuals seeking care at 1 of these facilities during 2017 were not included in the analysis.
As 1 of the few published studies of vasectomy and vasectomy reversal incidence among a large demographically diverse population of U.S. active component service men, this study makes a useful contribution to the literature on temporal changes in the incidence of these surgical procedures by age and race/ethnicity. Observed differences in incidence rates of vasectomy by service and military occupation warrant further analysis to examine adjusted (e.g., by age, race/ethnicity, and marital status) incidence rates among service members within these groups. In addition, further analysis of the sociodemographic characteristics of service men who underwent vasectomy and subsequent vasectomy reversal may help delineate factors impacting sterilization, which may help inform future pre-vasectomy counseling and thus patient choice.
References
- Philp T, Guillebaud J, Budd D. Complications of vasectomy: review of 16,000 patients. Br J Urol. 1984;56:745–748.
- Sharma V, Le BV, Sheth KR, et al. Vasectomy demographics and postvasectomy desire for future children: results from a contemporary national survey. Fertil Steril. 2013;99(7)1880–1885.
- Martinez GM, Chandra A, Abma JC, Jones J, Mosher WD. Fertility, contraception, and fatherhood: data on men and women from cycle 6 (2002) of the National Survey of Family Growth. National Center for Health Statistics. Vital Health Stat 23. 2006;(26):1–142.
- Eisenberg ML, Lipshultz LI. Estimating the number of vasectomies performed annually in the United States: data from the National Survey of Family Growth. J Urol. 2010;184(5):2068–2072.
- Ostrowski KA, Holt SK, Haynes B, Davies BJ, Fuchs EF, Walsh TJ. Evaluation of vasectomy trends in the United States. Urology. 2018;118:76–79.
- Khan AI, Patil D, Kawass JF, Zholudev V, Mehta A. Surgical sterilization among US men and women with employer-based insurance: a claims data analysis. Contraception. 2018;98(3):247–251.
- Barone MA, Hutchinson PL, Johnson CH, Hsia J, Wheeler J. Vasectomy in the United States, 2002. J Urol. 2006;176(1):232–236.
- Sharlip ID, Belker AM, Honig S, et al. Vasectomy: AUA guideline. J Urol. 2012;188(6 suppl):2482–2491.
- Johnson D, S JI. Vasectomy: tips and tricks. Transl Androl Urol. 2017;6(4)704–709.
- Cook LA, Pun A, van Vliet H, et al. Scalpel vs. no-scalpel incision for vasectomy. Cochrane Database Syst Rev. 2007;18:CD004112.
- Goldstein M. Vasectomy reversal. Compr Ther. 1993;19:37–41.
- Potts JM, Pasqualotto FF, Nelson D, et al. Patient characteristics associated with vasectomy reversal. J Urol. 1999;161:1835–1839.
- The Practice Committee of the American Society for Reproductive Medicine. Vasectomy reversal. Fertil Steril. 2004;82(suppl 1):S194–S198.
- Dickey RM, Pastuszak AW, Hakky TS, Chandrashekar A, Ramasamy R, Lipshultz LI. The evolution of vasectomy reversal. Curr Urol Rep. 2015;16(6):40.
- Nseyo U, Patel N, Hsieh TC. Vasectomy reversal surgical patterns: an analysis of the American Board of Urology case logs. Urology. 2017;107:107–113.
- Santomauro M, Masterson J, Marguet C, Crain D. Demographics of men receiving vasectomies in the U.S. military 2000–2009. Curr Urol. 2012;6(1):15–20.
- Masterson J, Avalos E, Santamauro M, et al. A retrospective review of factors associated with vasovasostomies in United States military members. Curr Urol. 2013;6(3)150–155.
- Anderson JE, Jamieson DJ, Warner L, Kissin DM, Nangia AK, Macaluso M. Contraceptive sterilization among married adults: national data on who chooses vasectomy and tubal sterilization. Contraception. 2012;85(6):552–557.
- Lamberts RW, Guo DP, Li S, Eisenberg ML. The relationship between offspring sex ratio and vasectomy utilization. Urology. 2017;103:112–116.
- Eisenberg ML, Henderson JT, Amory JK, Smith JF, Walsh TJ. Racial differences in vasectomy utilization in the United States: data from the National Survey of Family Growth. Urology. 2009;74(5):1020–1024.
- Borrero SB, Moore CG, Creinin MD, Ibrahim SA. Low rates of vasectomy among minorities: a result of differential receipt of counseling? Am J Mens Health. 2010;4(3):243–249.
- Bumpass LL, Thomson E, Godecker AL. Women, men, and contraceptive sterilization. Fertil Steril. 2000;73(5):937–946.
- Eeckhaut MCW. Marital status and female and male contraceptive sterilization in the United States. Fertil Steril. 2015;103(6):1509–1515.
- Khandwala YS, Zhang CA, Lu Y, Eisenberg ML. The age of fathers in the USA is rising: an analysis of 168,867,480 births from 1972 to 2015. Human Reprod. 2017;32(10):2110–2116.
- Shapiro DD, Kamnetz SA, Le BV. Vasectomy practice patterns among family medicine physicians and compliance with the American Urological Association 2012 Vasectomy Guidelines. Urology. 2017;109:115–120.
- Johnson D, Sandlow JI. Vasectomy: tips and tricks. Transl Androl Urol. 2017;6(4):704–709.
- TRICARE Covered Services. Assisted Reproductive Services. https://www.tricare.mil/CoveredServices/IsItCovered/AssistedReproductiveServices. Accessed 8 Feb. 2019.
- Howard G. Who asks for vasectomy reversal and why? Br Med J (Clin Res Ed). 1982;285(6340):490–492.
- Hendry WF. Vasectomy and vasectomy reversal. Br J Urol. 1994;73(4):337–344.
- Clarke L, Gregson S. Who has vasectomy reversal? J Biosoc Sci. 1986;18(3)253–259.
- Shah ZH, Ganta SB, Morgans BT. The trends of vasectomy reversal in the forces. J R Army Med Corps. 2003;149(4):265–266.
Key points
• The crude annual incidence rates of vasectomy among active component service men increased slightly over the course of the 18-year surveillance period; compared to their respective counterparts, higher overall incidence rates were observed among those aged 30–39 years, non-Hispanic white service men, married service men, and those in pilot/air crew occupations.
• Among the men who underwent incident vasectomy, 2.2% had another vasectomy performed during 2000–2017; 1.8% of those who underwent incident vasectomy also had at least 1 vasectomy reversal during this period.
• The likelihood of vasectomy reversal decreased with advancing age with half of the men undergoing the reversal procedure 2–5 years after the initial vasectomy; non-Hispanic black and Hispanic service men were more likely than those of other race/ethnicity groups to undergo vasectomy reversals.
Learning objectives
• The reader will explain how overall vasectomy incidence rates among active component service men compare to those in the U.S. civilian population.
• The reader will analyze overall and subgroup specific patterns in the incidence rates of vasectomy among active component service men in the U.S. Armed Forces.
• The reader will interpret data related to differences in the likelihood of vasectomy reversal among active component service men in different age and race/ethnicity groups.
Disclosures: MSMR editorial staff engage in a monthly collaboration with the DHA J7 Continuing Education Program Office (CEPO) to provide this CE/CME activity. MSMR staff authors, the DHA J7 CEPO, as well as the planners and reviewers of this activity have no financial or nonfinancial interest to disclose.