Abstract
The attrition of service members is a costly concern for the U.S. military and can lead to reduced readiness. While there have been studies identifying reasons for attrition, little is known about the relationship between perceived barriers to behavioral health care and attrition. A cross-sectional survey was conducted as part of a behavioral health epidemiological consultation at a U.S. Army division (n=5,842) during the COVID-19 pandemic in 2020. Odds of intending to leave the Army increased by 6% for each additional perceived barrier to behavioral health care. Soldiers’ concerns about the potential negative impacts on their careers or work environments were the most frequently cited barriers to behavioral health care.
What Are the New Findings?
This study found that 55% of surveyed soldiers intended to leave the Army at the end of their contract, and each additional perceived barrier to behavioral health care was associated with 6% higher odds of intentions to attrite. Soldiers who screened positive for depression or anxiety were also more likely to report intentions to leave the Army.
What Is the Impact on Readiness and Force Health Protection?
High levels of attrition result in high costs and lowered readiness. Soldiers with behavioral health conditions may intend to leave service for numerous reasons. To sustain readiness, the Army should dedicate resources to ensure soldiers have adequate access to behavioral health care and are not subject to stigma for accessing care for behavioral health concerns.
Background
Service member attrition within the first term of service ranges from 18.5% in the U.S. Marine Corps to 29.7% in the U.S. Army.1 First term attrition is a costly occurrence in the U.S. military with each instance costing from $15,000 to $25,000 to include training and equipment costs in the case of enlisted soldiers.1 Attrition is of particular concern to the military because of its negative impact on readiness and its potential to increase training costs. Although the costs of first term attrition have been quantified1, little is known about the factors that impact career attrition beyond the first term and before 20 years of service.
There is extensive knowledge about the impact of injuries and chronic diseases on military careers, but the knowledge about the behavioral health aspects of attrition is limited in comparison.2–6 One possible reason for early career attrition related to behavioral health concerns is insufficient access to, or perceived barriers to use of, behavioral health care resources. The Army has the highest reported burden of behavioral health conditions of all military branches.7–8 In 2016, 26% of active duty Army soldiers had a behavioral health diagnosis, such as a mood disorder or adjustment disorder, which is 6% higher than the average for service members across the 4 branches.7–8
Similar to civilians, soldiers may encounter barriers to accessing behavioral health care. Soldiers may perceive that seeking care for behavioral health needs will lead to career stagnation or will result in occupational stressors, such as being seen as weak, being treated differently, and difficulty getting time off for appointments. There is extensive literature demonstrating that seeking behavioral health care does not affect career trajectory, unless the behavioral health issue has already led to duty-limiting recommendations, the service member intends to commit a crime, or engages in conduct unbecoming.9–13
While there are previous studies of the relationship between stigma, help-seeking, and treatment outcomes, there is limited evidence on what impact service members’ perceived barriers to behavioral health care may have on early career attrition.4 Several studies have shown that the service members who report the highest perceived barriers to behavioral health care are also the ones who have the highest utilization of such services, presumably indicating a more severe condition or inability to get the treatment that they desire.7,14–16 A study published using data from a U.S Marine Corps sample found that Marines who sought treatment for behavioral health conditions were more likely to be separated from the military and have shorter lengths of service than Marines who did not seek such treatment.10,17 However, Marines who sought treatment for behavioral health conditions were not significantly more likely to be separated involuntarily, which indicates that most of the Marines in the study sample could have left of their own volition.10 Further investigation is warranted; therefore, the objective of this analysis was to examine the association between perceived barriers to behavioral health care and intentions to leave the Army after contract completion.
Methods
Study Population
This secondary analysis used survey data from a behavioral health epidemiological consultation conducted in 2020 by the U.S. Army Public Health Center’s Division of Behavioral and Social Health Outcomes Practice. The purpose of this behavioral health epidemiological consultation was to assess adverse behavioral and social health outcomes among soldiers following a perceived increase in suicide in an Army division, in addition to the potential exacerbating factors introduced by the COVID-19 pandemic. The survey included questions pertaining to demographics, Army career characteristics, COVID-19 health behaviors, food security, physical fitness, sleep, behavioral health, substance use, operational tempo, leadership, social support, behavioral health access and perceived barriers to care, and suicide ideation. Soldiers completed the survey in the summer of 2020. For the purpose of this secondary analysis, survey data (n=5,842 soldiers) on sociodemographic characteristics, Army career characteristics, and behavioral health characteristics were examined.
Main predictor and outcome
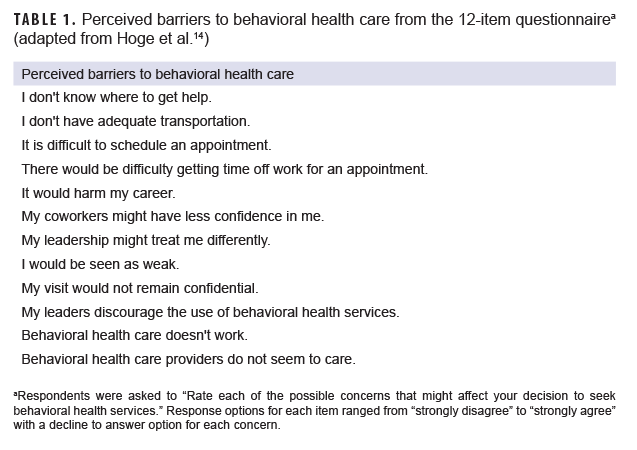
The main predictor was based on soldiers' responses to the question, "Rate each of the possible concerns that might affect your decision to seek behavioral health services" Twelve possible concerns were listed (adapted from Hoge et al. 2004; Table 1).18 The response options for each concern ranged from "strongly disagree" to "strongly agree" with a decline to answer option for each concern. Responses to each concern were dichotomized (strongly agree or agree=1; neutral, disagree, or strongly disagree=0; decline to answer was coded as missing) and then summed to create a total behavioral health care barrier concerns score (range: 0–12).
The main outcome was soldiers' intent to leave the Army after the current service period. Soldiers were asked their intentions to leave the Army after contract completion based on a 5-point Likert scale (very unlikely, somewhat unlikely, neither likely nor unlikely, somewhat likely, very likely, and decline to answer). Responses to this question were collapsed into 2 categories: yes (somewhat likely, very likely) and no (very unlikely, somewhat unlikely, neither likely nor unlikely). Decline to answer responses were coded as missing.
Sociodemographic and Army career characteristics
To assess the association between perceived barriers to behavioral health care and intentions to leave the Army, the analysis controlled for sociodemographic characteristics including sex; Hispanic origin (Hispanic and non-Hispanic); racial group (White/Caucasian, Black/African American, Asian/Pacific Islander, other/multiracial and unspecified race with Hispanic origin); marital status (married/in a relationship, separated/divorced/widowed, and single, never married); and parental status (children or no children). Racial group was based on responses to the question, "What is your race/ethnicity? Select all that apply". The response options included 1) White, 2) Black or African American, 3) Asian/Pacific Islander, 4) Hispanic, Latino, or Spanish Origin, or 5) other race, ethnicity, or origin. Soldiers who only selected "other race, ethnicity or origin" were classified as "other". Soldiers who selected more than one racial group were classified as "multiracial." "Multiracial" and "other" categories were combined because of small cell sizes. Soldiers who selected "Hispanic, Latino, or Spanish origin" without indicating whether they were White, Black, Asian/Pacific Islander, or other were classified as "Unspecified race with Hispanic origin." This was done to distinguish this group from soldiers who did not provide a response to this question. Soldiers who selected "Hispanic, Latino, or Spanish Origin," regardless whether they were White, Black, Asian/Pacific Islander, or other, were classified as "Hispanic." Soldiers who did not select "Hispanic, Latino, or Spanish Origin," but indicated that they were White, Black, Asian/Pacific Islander, or other, were classified as "non-Hispanic."
Army career characteristics included rank (junior enlisted [E1–E4], junior noncommissioned officer [E5–E6], senior noncommissioned officer [E7–E9], junior commissioned officer [O1–O3], senior commissioned officer [O4 or above], and warrant officer [WO1–CW5]) and job satisfaction. Although E4s are classified as junior enlisted, certain E4s (corporals) are also considered junior non-commissioned officers. For the purposes of this study, no distinction was made between specialists and corporals. Job satisfaction was assessed using the survey question, "How satisfied are you with your job overall?" with a 5-point Likert scale ranging from very satisfied to very dissatisfied. For this analysis, job satisfaction was collapsed into 3 categories including satisfied, neutral, or dissatisfied.
Behavioral health characteristics
Depression and anxiety were assessed using the 4-item Patient Health Questionnaire (PHQ-4).19
The first 2 questions of this tool measure anxiety and the last 2 questions measure depression. Composite scores of negative (0–2) and positive (3–6) were used for each condition. Post-traumatic stress disorder (PTSD) was assessed using the PTSD Checklist Civilian Version 2 (PCL-C2) with composite scores of 0–3 coded as negative and 4–8 as positive.20
Resilience (low [1.00–2.99], normal [3.00–4.30], and high [4.31–5.00]) was measured using the average score of 6 questions from the Brief Resilience Scale.21
The analysis also controlled for current access to behavioral health services (e.g., unit or garrison chaplain, behavioral health officer, Substance Use Disorder Clinical Care program, psychologist, psychiatrist, and licensed counselor) (yes/no). On the survey, this question was asked immediately before asking about perceived behavioral health care barriers.
Statistical analysis
Soldiers with missing responses on any covariate were excluded from the analysis. To descriptively compare the overall study population and the analytic sample, both sets of demographics and military characteristics were analyzed. Due to the analytic sample nesting within the overall study population (i.e., not mutually exclusive), no statistical tests were performed. Multivariable logistic regression was used to determine the association between the perceived behavioral health care barriers score and intentions to leave the Army after contract completion, adjusting for sociodemographic, Army career, and behavioral health characteristics. Adjusted odd ratios (AORs) and their 95% confidence intervals (CIs) were calculated for each variable. The regression model was built in 1 step, and all predictors were selected a priori based on existing literature. All analyses were completed using SAS, version 9.4 (SAS Institute, Cary, NC). The alpha to determine statistical significance was set at p<.05.
Results
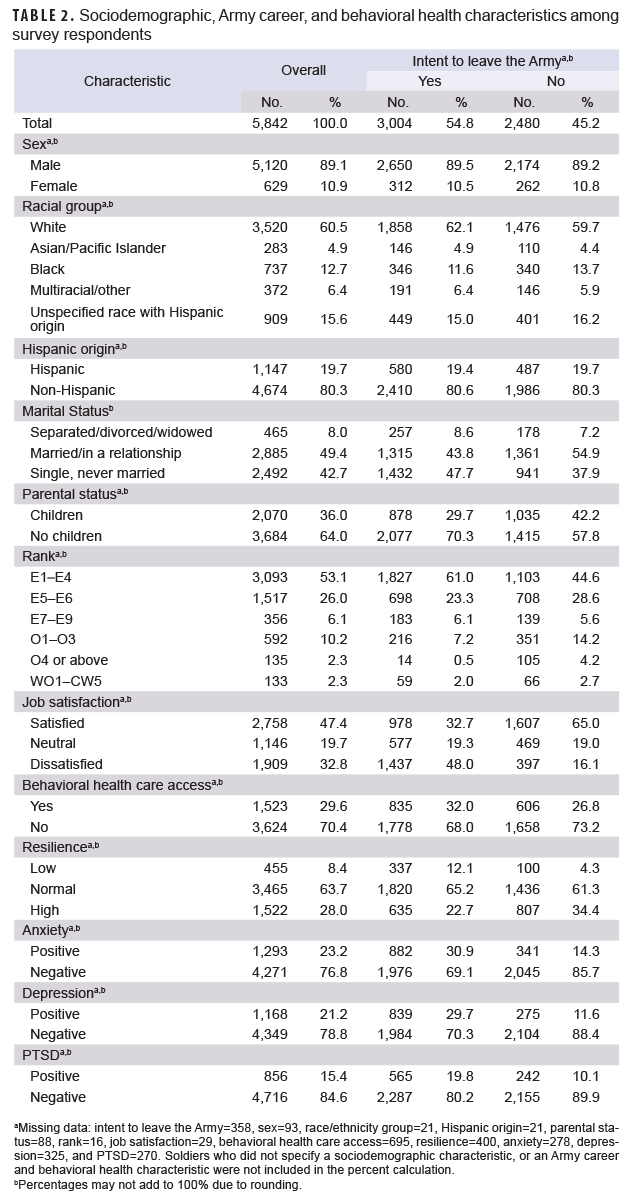
A total of 5,842 soldiers were surveyed (5,120 men, 629 women, 93 sex unspecified) (Table 2). Of the 5,484 respondents with data on the main outcome, approximately 55% had intentions to leave the Army after contract completion. Of those with intent to leave, the majority were White (62%), non-Hispanic (81%), junior enlisted (61%), and without children (70%); had normal resilience (65%), and were not accessing behavioral health services at the time of the survey (68%). Nearly half of respondents with intentions to leave the Army were single, never married (48%) or dissatisfied with their jobs (48%). The most commonly perceived barriers to behavioral health care were related to stigma (data not shown). On average, soldiers reported 2 out of 12 behavioral health care concerns (median=1.0; standard deviation=2.8) (data not shown). The majority of soldiers with an intent to leave the Army screened negative for anxiety (69%), depression (70%), or PTSD (80%) (Table 2).
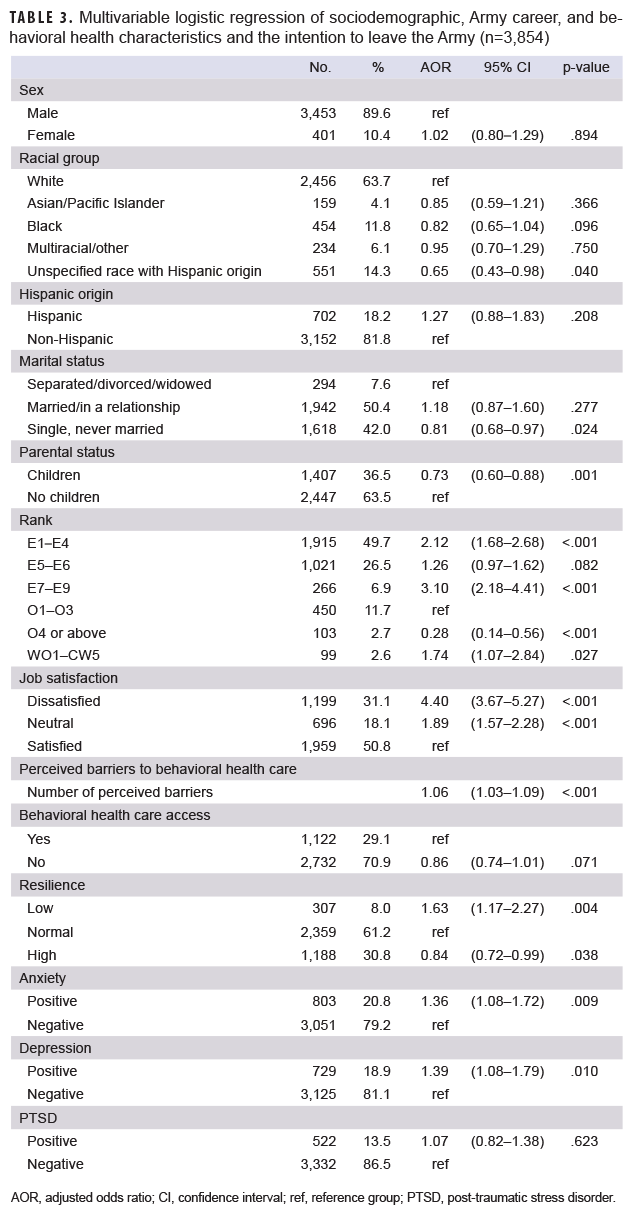
A total of 3,854 respondents (66% of the full sample) with complete information on the covariates were included in the logistic regression analysis (Table 3). The analytic sample was descriptively similar to the overall study population in terms of demographic and military characteristics. The odds of a soldier intending to leave the Army increased by 6% for each additional perceived barrier to behavioral health care, after adjusting for covariates. Soldiers with a rank of major (O4) and above (AOR=0.28; 95% CI: 0.14–0.56) were less likely to intend to leave the Army compared to soldiers in other rank groups. Soldiers who reported they were dissatisfied with their jobs (AOR=4.40; 95% CI: 3.67–5.27) had odds of intention to leave the Army that were 4.4 times that of those who reported being satisfied with their jobs (Table 3). For soldiers who screened positive for anxiety or depression, odds of leaving the Army were 36% and 39% higher, respectively, than those who screened negative for these conditions (AOR=1.36; 95% CI: 1.08–1.72 and AOR=1.39; 95% CI: 1.08–1.79, respectively). There was no association between behavioral health care access at the time of the survey and soldiers’ intentions to leave the Army (p=.07).
Editorial Comment
Attrition in the military is a multifaceted issue that can have wide-ranging, long-lasting effects. High levels of attrition result in high costs and lowered readiness. The factors that influence decisions to leave the military prior to 20 years of service are not well understood. Survey results demonstrated that 55% of the surveyed soldiers intended to leave the Army at the end of their current contract. Additionally, each additional reported perceived barrier to behavioral health care was associated with 6% higher odds of intentions to leave. Soldiers who screened positive for depression or anxiety were also more likely to report intentions to leave compared to those who screened negative for these conditions. The findings also indicate that job satisfaction and being a senior officer are both potential protective factors for attrition.
This study had notable limitations. The sample used in this study was from 1 Army division and may not have been representative of the entire Army. Second, this sample did not distinguish between the 2 E4 pay grades (specialist and corporal). As a result, the findings did not capture potential differences between these 2 groups. Third, although no identifying information was collected, social desirability bias (i.e., the tendency to underreport socially undesirable attitudes/behaviors) could have been present leading to an attenuation of reporting barriers to behavioral health care. Fourth, it is also possible that the healthy warrior effect resulted in selection bias for the sample. The healthy warrior effect states that there is a disproportionate loss of psychologically unfit personnel early in training, which is amplified by numerous efforts to screen out as many individuals as possible prior to enlistment or commissioning.22 Fifth, it is also possible that the results are skewed due to an already existing issue in this specific population since behavioral health epidemiological consultations are only requested by units who have a perceived increase in social or behavioral health conditions. The pre-existing social, behavioral health, or organizational environment concerns within this division that were not measured by this study, including from the COVID-19 pandemic, could have contributed to intentions to leave the Army. Sixth, the analytic sample included individuals who may intend to leave the Army after the current service contract primarily because they are eligible for retirement (e.g., 20 years of service). However, results of the bivariate analyses indicated that respondents who were senior in ranks (i.e., O4 and above, E7 and above) were less likely to intend to attrite than other rank groups. Lastly, given that this was a cross-sectional study, no conclusions about causality can be drawn. The strengths of this study included a large sample within the Army and the minimization of social desirability bias since the survey was self-directed and anonymous.
The findings of the current study point to numerous potential areas for future investigation. The COVID-19 pandemic has had a significant impact on behavioral health and continues to affect the psychological well-being of individuals worldwide.23–26 Previous studies have shown the pandemic exacerbated already existing racial disparities, loneliness, and strained social support systems, especially as a result of the restrictions put in place to reduce the spread of COVID-19.23–29 While the effects of the pandemic on the results of this study are unknown, it is likely that the results were biased away from the null due to COVID-19.
One of the most commonly reported barriers to seeking or receiving behavioral health care in military populations is stigma. In this study, 6 stigma specific questions were incorporated into the 12-item questionnaire on barriers to behavioral health care. Although race and ethnicity did not significantly impact the intention to leave the Army (except for unspecified race with Hispanic origin), elucidating racial disparities in perceived stigma could be a future direction. 30
Another important area to address is the number of behavioral health care providers in the military.31,32
A 2010 report by the Department of Defense found that a dearth of providers made it difficult for service members to seek care and led to negative outcomes, such as suicidal behavior.33
Subsequent studies found that the number of providers has not increased in the years since.34–37
The most persistent barriers continue to be the stigma associated with seeking behavioral health care.9,14,38,39
To ensure that readiness is maintained and soldiers maintain holistic health, additional resources need to be dedicated to making sure soldiers have adequate access to, and perceive little stigma when seeking, behavioral health care resources.
Affiliations: Division of Behavioral and Social Health Outcomes Practice, U.S. Army Public Health Center, Aberdeen Proving Ground, MD (Ms. Kaplansky, Ms. Ackah-Toffey, Dr. Beymer, and Dr. Schaughency); Oak Ridge Institute for Science and Education, Oak Ridge, TN (Ms. Kaplansky); General Dynamics Information Technology Inc., Falls Church, VA (Ms. Ackah-Toffey).
Disclaimer: The views expressed in this publication are those of the authors and do not necessarily reflect the official policy or position of the U.S. Department of the Army, the U.S. Department of Defense, or the U.S. Government.
Human research protection: The Public Health Review Board of the U.S. Army Public Health Center determined this activity to be public health practice under 21-960.
Project support: This project was supported in part by an appointment to the Research Participation Program for the U.S. Army Public Health Center administered by the Oak Ridge Institute for Science and Education through an agreement between the U.S. Department of Energy and the U.S. Army Public Health Center.
References
- Marrone JV. Predicting 36-month attrition in the U.S. military: A comparison across service branches. Santa Monica, CA: RAND Corporation; 2020. Accessed 30 August 2021.
-
https://www.rand.org/pubs/research_reports/RR4258.html
- Schwartz O, Libenson T, Astman N, Haim L. Attrition due to orthopedic reasons during combat training: Rates, types of injuries, and comparison betwen infantry and noninfantry units. Mil Med. 2014;179(8):897–900.
- Molloy JM, Pendergrass TL, Lee IE, Chervak MC, Hauret KG, Rhon DI. Musculoskeletal injuries and United States Army readiness Part I: Overview of injuries and their strategic impact. Mil Med. 2020;185(9–10).
- Garcia SMS, Ortman BV, Burnett DG. Mental health diagnoses and attrition in Air Force recruits. Mil Med. 2015;180(4):436–444.
- Garvey Wilson AL, Messer SC, Hoge CW. U.S. military mental health care utilization and attrition prior to the wars in Iraq and Afghanistan. Soc Psychiatry Psychiatr Epidemiol. 2009;44(6):473–481.
-
Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295(9):1023–1032.
-
Deployment Health Clinical Center. Mental Health Care Utilization by Active Duty Service Members in the Military Health System, Fiscal Years 2005–2016. Falls Church, VA; 2017. Accessed 30 August 2021. https://www.pdhealth.mil/sites/default/files/images/mental-health-care-utilization-among-active-duty-service-members-508.pdf
-
Deployment Health Clinical Center. Mental Health Disorder Prevalence and Incidence among Active Duty Service Members, 2005–2017. Falls Church, VA; 2019. Accessed 30 August 2021. https://www.pdhealth.mil/sites/default/files/images/mental-health-disorder-prevalence-among-active-duty-service-members-508.pdf
-
Hom MA, Stanley IH, Schneider ME, Joiner TE. A systematic review of help-seeking and mental health service utilization among military service members. Clin Psychol Rev. 2017;53:59–78.
-
Ghahramanlou-Holloway M, LaCroix J, Koss K, et al. Outpatient mental health treatment utilization and military career impact in the United States Marine Corps. Int J Environ Res Public Health. 2018;15(4):828.
-
Ghahramanlou-Holloway M, Koss K, Rowan A, et al. Retrospective and prospective examination of outpatient mental health utilization and military career impacts. Stigma Health. 2019;4(2):143–151.
-
Cerully JL, Acosta JD, Sloan J. Mental health stigma and its effects on treatment-related outcomes: A narrative review. Mil Med. 2018;183(11–12):e427–e437.
-
Varga CM, Haibach MA, Rowan AB, Haibach JP. Psychiatric history, deployments, and potential impacts of mental health care in a combat theater. Mil Med. 2017;183(1–2):e77–e82.
-
Bryan CJ, Wood D, Applegarth M, Bryan ABO. Subtypes of mental health stigma and barriers to care among National Guard personnel: Results of a latent class analysis. Armed Forces Soc. 2020;46(3):424–437.
-
Boulos D, Zamorski MA. Do shorter delays to care and mental health system renewal translate into better occupational outcome after mental disorder diagnosis in a cohort of Canadian military personnel who returned from an Afghanistan deployment? BMJ Open. 2015;5(12):e008591.
-
Rosellini AJ, Stein MB, Benedek DM, et al. Using self-report surveys at the beginning of service to develop multi-outcome risk models for new soldiers in the U.S. Army. Psychol Med. 2017;47(13):2275–2287.
- Zuromski KL, Dempsey CL, Ng THH, et al. Utilization of and barriers to treatment among suicide decedents: Results from the Army Study to Assess Risk and Resilience Among servicemembers (Army STARRS). J Consult Clin Psychol. 2019;87(8):671–683.
-
Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351(1):13–22.
-
Löwe B, Wahl I, Rose M, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122(1–2):86–95.
-
Lang AJ, Stein MB. An abbreviated PTSD checklist for use as a screening instrument in primary care. Behav Res Ther. 2005;43(5):585–594.
-
Smith BW, Epstein EM, Ortiz JA, Christopher PJ, Tooley EM. The Foundations of Resilience: What Are the Critical Resources for Bouncing Back from Stress? In: Prince-Embury S, Saklofske
eds. Resilience in Children, Adolescents, and Adults. The Springer Series on Human Exceptionality. Springer, New York, NY; 2013:167–187.
-
Larson GE, Highfill-McRoy RM, Booth-Kewley S. Psychiatric diagnoses in historic and contemporary military cohorts: combat deployment and the healthy warrior effect. Am J Epidemiol. 2008;167(11):1269–1276.
-
Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 2020;3(9):e2019686.
-
Salari N, Hosseinian-Far A, Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020;16(1):57.
-
Usher K, Durkin J, Bhullar N. The COVID-19 pandemic and mental health impacts. Int J Ment Health Nurs. 2020;29(3):315–318.
-
Cullen W, Gulati G, Kelly BD. Mental health in the COVID-19 pandemic. QJM. 2020;113(5):311–312.
-
Selden TM, Berdahl TA. COVID-19 and racial/ethnic disparities in health risk, employment, and household composition. Health Aff (Millwood). 2020;39(9):1624–1632.
-
Gravlee CC. Systemic racism, chronic health inequities, and COVID-19: A syndemic in the making? Am J Hum Biol. 2020;32(5):e23482.
-
Gross CP, Essien UR, Pasha S, Gross JR, Wang SY, Nunez-Smith M. Racial and ethnic disparities in population-level COVID-19 mortality. J Gen Intern Med. 2020;35(10):3097–3099.
-
Chu KM, Garcia SMS, Koka H, Wynn GH, Kao TC. Mental health care utilization and stigma in the military: comparison of Asian Americans to other racial groups. Ethn Health. 2021;26(2):235–250.
-
Russell MC, Schaubel SR, Figley CR. The darker side of military mental health care part one: Understanding the military’s mental health dilemma. Psychol Inj Law. 2018;11(1):22–36.
-
Russell MC, Schaubel SR, Figley CR. The darker side of military mental health care part Two: Five harmful strategies to manage its mental health dilemma. Psychol Inj Law. 2018;11(1):37–68.
-
Defense Health Board. The Challenge and the Promise: Strengthening the Force, Preventing Suicide and Saving Lives. Final Report of the Department of Defense Task Force on the Prevention of Suicide by Members of the Armed Forces. Washington, DC: United States of America, Dept. of Defense; 2010. Accessed 30 August 2021. https://apps.dtic.mil/sti/citations/ADA529502
-
Health Resources and Services Administration. Bureau of Health Workforce. National Center for Health Workforce Analysis. National projections of supply and demand for selected behavioral health practitioners: 2013–2025. Rockville, MD; 2016. Accessed 30 August 2021. https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/behavioral-health-2013-2025.pdf
-
U.S. Department of Defense. Office of the Inspector General. Access to care at selected military treatment facilities. Alexandria, VA; 2018. Accessed 30 August 2021. https://media.defense.gov/2018/May/16/2001917965/-1/-1/1/DODIG-2018-111.PDF
-
U.S. Department of Defense. Office of the Inspector General. Evaluation of access to mental health care in the Department of Defense. Alexandria, VA; 2020. Accessed 30 August 2021. https://media.defense.gov/2020/Aug/12/2002475605/-1/-1/1/DODIG-2020-112_REDACTED.PDF
- Office of the Under Secretary of Defense for Personnel and Readiness. Report to Congressional Armed Services Committees. House Report 115-676. Mental Health Care in the Military Health System; 2019. Accessed 30 August 2021. https://health.mil/Reference-Center/Congressional-Testimonies/2019/05/24/Mental-Health-Care-in-the-MHS.
- Gardiner F, Gardiner EC. Similarities between military and medical service: stigma of seeking mental health assistance. BMJ Mil Health. 2020;166(3):181–182.
- Tanielian T, Woldetsadik MA, Jaycox LH, et al. Barriers to engaging service members in mental health care within the U.S. military health system. Psychiatr Serv. 2016;67(7):718–727.