Surveillance Snapshot: Incidence of Rickettsial Diseases Among Active and Reserve Component Service Members, U.S. Armed Forces, 2010–2018
 Dorsal view of a female American dog tick, Dermacentor variabilis. Credit: CDC/Gary O. Maupin
Dorsal view of a female American dog tick, Dermacentor variabilis. Credit: CDC/Gary O. Maupin
Rickettsial diseases are vector-borne, bacterial infections that cause acute febrile illness throughout the world. Because symptoms of rickettsial diseases are often non-specific in nature and overlap with other febrile diseases with similar epidemiology, their diagnosis is challenging. The diagnostic difficulties likely contribute to the historical underreporting of cases of these diseases.
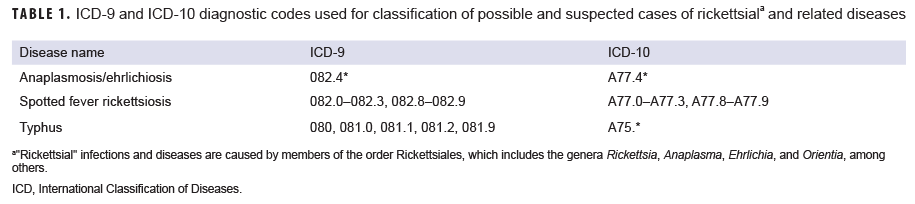
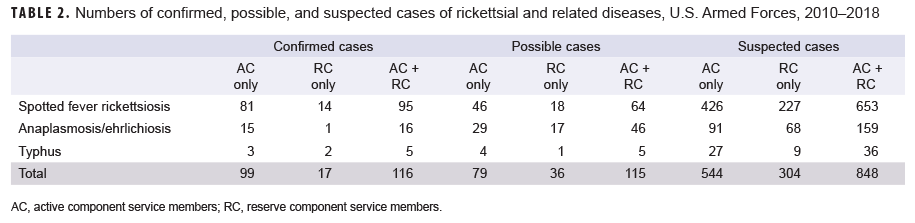
In 2018, the MSMR published a report on the surveillance of vector-borne disease in active and reserve component service members that included estimates of incident cases of rickettsial and related diseases during the surveillance period from 2010 through 2016.1 The analysis for this snapshot used similar methodology but restricted the analysis to rickettsial diseases and extended the surveillance period through 2018. A "confirmed" case was defined as an individual identified through a reportable medical event (RME) report of a rickettsial or related disease that was described as "confirmed" by having met specific laboratory and/or epidemiologic criteria.2 A "possible" case was defined by a record of hospitalization with a diagnosis for a rickettsial disease (Table 1) in any diagnostic position. A "suspected" case was defined by either an RME of a rickettsial disease without laboratory or epidemiologic confirmation or a record of an outpatient medical encounter with a diagnosis of a rickettsial disease in the first or second diagnostic position. An individual could be counted once per lifetime for each type of rickettsial disease. Individuals diagnosed as a case before the start of the surveillance period were excluded. Confirmed cases were prioritized over possible and suspected cases, respectively (Table 2).
These data indicate that a continued multidisciplinary focus on preventive measures to counter the threat of these diseases is warranted. Most important are effective vector control and adherence to personal protective measures.
References
- O'Donnell FL, Stahlman S, Fan M. Surveillance for vector-borne diseases among active and reserve component service members, U.S. Armed Forces, 2010–2016. MSMR. 2018;25(2):8–15.
- Defense Health Agency. Armed Forces Health Surveillance Branch. Armed Forces Reportable Medical Events. Guidelines and Case Definitions, 2017. https://health.mil/reference-Center/Publications/2017/07/17/Armed-Forces-Reportable-Medical-Events-Guidelines. Accessed 17 July 2019.
You also may be interested in...
Article
Feb 1, 2019
Glaucoma is an eye disease that involves progressive optic nerve damage and vision loss, leading to blindness if undetected or untreated. This report describes an analysis using the Defense Medical Surveillance System to identify all active component service members with an incident diagnosis of glaucoma during the period between 2013 and 2017. The ...
Article
Feb 1, 2019
The MSMR has been publishing the results of surveillance studies of malaria since 1995. The standard MSMR case definition uses Medical Event Reports and records of hospitalizations in counting cases of malaria. This report summarizes the performance of the standard MSMR case definition in estimating incident cases of malaria from 2015 through 2017. ...
Article
Feb 1, 2019
Human adenoviruses (HAdVs) are known to cause respiratory illness outbreaks at basic military training (BMT) sites. HAdV type-4 and -7 vaccines are routinely administered at enlisted BMT sites, but not at military academies. During Aug.–Sept. 2016, U.S. Naval Academy clinical staff noted an increase in students presenting with acute respiratory ...
Article
Dec 1, 2018
This analysis describes the incidence and prevalence of five thyroid disorders (goiter, thyrotoxicosis, primary/not otherwise specified [NOS] hypothyroidism, thyroiditis, and other disorders of the thyroid) among active component service members between 2008 and 2017. During the 10-year surveillance period, the most common incident thyroid disorder ...
Article
Dec 1, 2018
This report uses ICD-9 and ICD-10 codes (277.7 and E88.81, respectively) for the metabolic syndrome (MetS) to summarize trends in the incidence and prevalence of this condition among active component members of the U.S. Armed Forces between 2002 and 2017. During this period, the crude overall incidence rate of MetS was 7.5 cases per 100,000 person ...
Article
Dec 1, 2018
During 2002–2017, the most common incident adrenal gland disorder among male and female service members was adrenal insufficiency and the least common was adrenomedullary hyperfunction. Adrenal insufficiency was diagnosed among 267 females (crude overall incidence rate: 8.2 cases per 100,000 person-years [p-yrs]) and 729 males (3.9 per 100,000 p-yrs). ...
Fact Sheet
Mar 30, 2017
 .PDF |
267.04 KB
.PDF |
267.04 KB
This fact sheet provides details on heat illnesses by location during a five-year surveillance period from 2012 through 2016. 11,967 heat-related illnesses were diagnosed at more than 250 military installations and geographic locations worldwide. Three Army Installations accounted for close to one-third of all heat illnesses during the period.
Fact Sheet
Mar 30, 2017
 .PDF |
313.80 KB
.PDF |
313.80 KB
This fact sheet provides details on Rhabdomyolysis by location for active component, U.S. Armed Forces during a five-year surveillance period from 2012 through 2016. The medical treatment facilities at nine installations diagnosed at least 50 cases each and, together approximately half (49.9%) of all diagnosed cases.
Fact Sheet
Mar 30, 2017
 .PDF |
283.00 KB
.PDF |
283.00 KB
This fact sheet provides details on the demographic and military traits of service members diagnosed as traumatic brain injury (TBI) cases during a 16-year surveillance period from 2001 through 2016, a total of 276,858 active component service members received first-time diagnoses of TBI - a structural alteration of the brain or physiological ...
You are leaving Health.mil
The appearance of hyperlinks does not constitute endorsement by the Department of Defense of non-U.S. Government sites or the information, products, or services contained therein. Although the Defense Health Agency may or may not use these sites as additional distribution channels for Department of Defense information, it does not exercise editorial control over all of the information that you may find at these locations. Such links are provided consistent with the stated purpose of this website.
You are leaving Health.mil
View the external links disclaimer.
Last Updated: July 11, 2023