Abstract
In 2018, there were 578 incident diagnoses of heat stroke and 2,214 incident diagnoses of heat exhaustion among active component service members. The overall crude incidence rates of heat stroke and heat exhaustion diagnoses were 0.45 cases and 1.71 cases per 1,000 person-years, respectively. In 2018, subgroup-specific rates of incident heat stroke diagnoses were highest among males and service members less than 20 years old, Asian/Pacific Islanders, Marine Corps and Army members, recruit trainees, and those in combat-specific occupations. Subgroup-specific incidence rates of heat exhaustion diagnoses in 2018 were notably higher among service members less than 20 years old, Asian/Pacific Islanders, Army and Marine Corps members, recruit trainees, and service members in combat-specific occupations. During 2014–2018, a total of 325 heat illnesses were documented among service members in Iraq and Afghanistan; 8.6% (n=28) were diagnosed as heat stroke. Commanders, small unit leaders, training cadre, and supporting medical personnel must ensure that the military members whom they supervise and support are informed about the risks, preventive countermeasures, early signs and symptoms, and first-responder actions related to heat illnesses.
What Are the New Findings?
Annual rates of incident heat stroke diagnoses increased steadily between 2014 and 2018. During the same period, the annual incidence rate of heat exhaustion diagnoses peaked in 2018. A sizable proportion of heat stroke and heat exhaustion cases identified through records of ambulatory visits did not prompt mandatory reports through the Reportable Medical Events System.
What Is the Impact on Readiness and Force Health Protection?
Heat illnesses can degrade U.S. military effectiveness by causing considerable morbidity, particularly during training of recruits and of soldiers and Marines in combat arms specialties. Complete and timely submission of mandatory reports of heat illness events ensures that local public health and command leaders have ready access to real-time surveillance data to identify trends and to guide preventive measures.
Background
Heat illness refers to a group of disorders that occur when the elevation of core body temperature surpasses the compensatory limits of thermoregulation.1 Heat illness is the result of environmental heat stress and/or exertion and represents a set of conditions that exist along a continuum from less severe (heat exhaustion) to potentially life threatening (heat stroke).
Heat exhaustion is caused by the inability to maintain adequate cardiac output because of strenuous physical exertion and environmental heat stress.1,2 Acute dehydration often accompanies heat exhaustion but is not required for the diagnosis.3 The clinical criteria for heat exhaustion include a core body temperature greater than 100.5ºF/38ºC and less than 104ºF/40ºC at the time of or immediately after exertion and/or heat exposure, physical collapse at the time of or shortly after physical exertion, and no significant dysfunction of the central nervous system. If any central nervous system dysfunction develops with heat exhaustion (e.g., dizziness or headache), it is mild and rapidly resolves with rest and cooling measures (e.g., removal of unnecessary clothing, relocation to a cooled environment, and oral hydration with cooled, slightly hypotonic solutions).1–4
Heat stroke is a debilitating illness characterized clinically by severe hyperthermia (i.e., a core body temperature of 104ºF/40ºC or greater), profound central nervous system dysfunction (e.g., delirium, seizures, or coma), and additional organ and tissue damage.1,4,5 The onset of heat stroke requires aggressive clinical treatments, including rapid cooling and supportive therapies such as fluid resuscitation to stabilize organ function.1,5 The observed pathologic changes in several organ systems are thought to occur through a complex interaction between heat cytotoxicity, coagulopathies, and a severe systemic inflammatory response.1,5 Multi-organ system failure is the ultimate cause of mortality due to heat stroke.5
Timely medical intervention can prevent milder cases of heat illness (e.g., heat exhaustion) from becoming severe (e.g., heat stroke) and potentially life threatening. However, even with medical intervention, heat stroke may have lasting effects, including damage to the nervous system and other vital organs and decreased heat tolerance, making an individual more susceptible to subsequent episodes of heat illness.6–8 Furthermore, the continued manifestation of multi-organ system dysfunction after heat stroke increases patients' risk of mortality during the ensuing months and years.9,10
Strenuous physical activity for extended durations in occupational settings as well as during military operational and training exercises exposes service members to considerable heat stress because of high environmental heat and/or a high rate of metabolic heat production.11 In some military settings, wearing needed protective clothing or equipment may make it biophysically difficult to dissipate body heat. The resulting body heat burden and associated cardiovascular strain reduce exercise performance and increase the risk of heat-related illness.11,12
Over many decades, lessons learned during military training and operations in hot environments as well as a substantial body of literature have resulted in doctrine, equipment, and preventive measures that can significantly reduce the adverse health effects of military activities in hot weather.13–19 Although numerous effective countermeasures are available, heat-related illness remains a significant threat to the health and operational effectiveness of military members and their units and accounts for considerable morbidity, particularly during recruit training in the U.S. military.11,20
In the U.S. Military Health System (MHS), the most serious types of heat-related illness are considered notifiable medical events. Notifiable cases of heat illness include heat exhaustion and heat stroke. All cases of heat illness that require medical intervention or result in change of duty status are reportable.4
This report summarizes reportable medical events of heat illness as well as heat illness-related hospitalizations and ambulatory visits among active component service members during 2018 and compares them to the previous 4 years. Episodes of heat stroke and heat exhaustion are summarized separately.
Methods
The surveillance period was 1 Jan. 2014 through 31 Dec. 2018. The surveillance population included all individuals who served in the active component of the Army, Navy, Air Force, or Marine Corps at any time during the surveillance period. All data used to determine incident heat illness diagnoses were derived from records routinely maintained in the Defense Medical Surveillance System (DMSS). These records document both ambulatory encounters and hospitalizations of active component service members of the U.S. Armed Forces in fixed military and civilian (if reimbursed through the MHS) treatment facilities worldwide. In-theater diagnoses of heat illness were identified from medical records of service members deployed to Southwest Asia or the Middle East and whose health care encounters were documented in the Theater Medical Data Store (TMDS). Because heat illnesses represent a threat to the health of individual service members and to military training and operations, the Armed Forces require expeditious reporting of these reportable medical events through any of the service-specific electronic reporting systems; these reports are routinely transmitted and incorporated into the DMSS.
For this analysis, a case of heat illness was defined as an individual with 1) a hospitalization or outpatient medical encounter with a primary (first-listed) or secondary (second-listed) diagnosis of heat stroke (International Classification of Diseases, 9th Revision [ICD-9]: 992.0; International Classification of Diseases, 10th Revision [ICD-10]: T67.0*) or heat exhaustion (ICD-9: 992.3–992.5; ICD-10: T67.3*–T67.5*) or 2) a reportable medical event record of heat exhaustion or heat stroke.21 Because of an update to the Disease Reporting System internet (DRSi) medical event reporting system in July 2017, the type of reportable medical events for heat illness (i.e., heat stroke or heat exhaustion) could not be distinguished using reportable medical event records in DMSS data. Instead, information on the type of reportable medical event for heat illness during the entire 2014–2018 surveillance period was extracted from the DRSi by the Defense Health Agency (DHA) Army Satellite and Army Public Health Center Staff.
It is important to note that previous MSMR analyses included diagnosis codes for other and unspecified effects of heat and light (ICD-9: 992.8 and 992.9; ICD-10: T67.8* and T67.9*) within the heat illness category "other heat illnesses." These codes were excluded from the current analysis and the April 2018 MSMR analysis. If an individual had a diagnosis for both heat stroke and heat exhaustion during a given year, only 1 diagnosis was selected, prioritizing heat stroke over heat exhaustion. Encounters for each individual within each calendar year then were prioritized in terms of record source, with hospitalizations prioritized over reportable events, which were prioritized over ambulatory visits.
For surveillance purposes, a "recruit trainee" was defined as an active component service member (grades E1–E4) who was assigned to 1 of the services' 9 recruit training locations (per the individual's initial military personnel record). For this report, each service member was considered a recruit trainee for the period corresponding to the usual length of recruit training in his or her service. Recruit trainees were considered a separate category of enlisted service members in summaries of heat illnesses by military grade overall.
Records of medical evacuations from the U.S. Central Command (CENTCOM) area of responsibility (AOR) (e.g., Iraq or Afghanistan) to a medical treatment facility outside the CENTCOM AOR were analyzed separately. Evacuations were considered case defining if affected service members had at least 1 inpatient or outpatient heat illness medical encounter in a permanent military medical facility in the U.S. or Europe from 5 days before to 10 days after their evacuation dates.
Medical data from military treatment facilities that are using MHS GENESIS are not available in the DMSS, which was implemented at different sites throughout 2017. These sites include Naval Hospital Oak Harbor, Naval Hospital Bremerton, Air Force Medical Services Fairchild, and Madigan Army Medical Center. Therefore, medical encounter data for individuals seeking care at any of these facilities during 2017–2018 were not included in this analysis.
Results
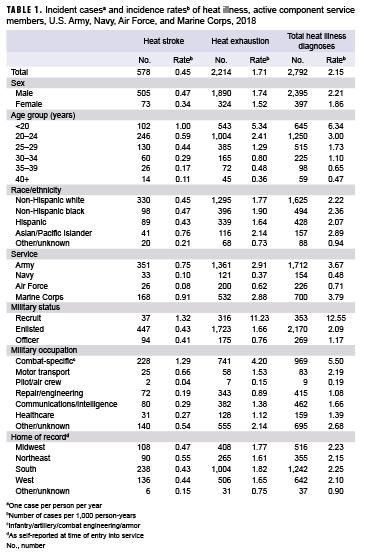
In 2018, there were 578 incident cases of heat stroke and 2,214 incident cases of heat exhaustion among active component service members (Table 1). The crude overall incidence rates of heat stroke and heat exhaustion diagnoses were 0.45 cases and 1.71 cases per 1,000 person-years (p-yrs), respectively. In 2018, subgroup-specific incidence rates of heat stroke diagnoses were highest among males, those less than 20 years old, Asian/Pacific Islanders, Marine Corps and Army members, recruit trainees, and those in combat-specific occupations (Table 1). The rate of incident heat stroke diagnoses was 20.9% higher among service members in the Marine Corps than among those in the Army; the Army rate was more than 7-fold the Navy rate and 9-fold the Air Force rate; and the rate among females was 26.5% lower than the rate among males. There were only 37 cases of heat stroke reported among recruit trainees, but their incidence rate was more than 3 times that of other enlisted members and officers.
Similar to the heat stroke findings, the crude overall incidence rate of heat exhaustion diagnoses among males was slightly higher than among females (Table 1). In 2018, subgroup-specific rates of incident heat exhaustion diagnoses were notably higher among service members less than 20 years old, Asian/Pacific Islanders, Army and Marine Corps members, recruit trainees, and service members in combat-specific occupations.
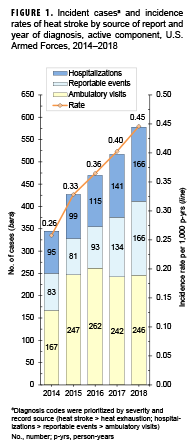
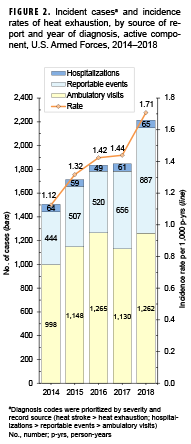
Crude (unadjusted) annual incidence rates of heat stroke diagnoses increased steadily from 0.26 cases per 1,000 p-yrs in 2014 to 0.45 cases per 1,000 p-yrs in 2018 (Figure 1). In 2018, there were more heat stroke-related hospitalizations and reportable medical events than in 2017 but similar numbers of ambulatory visits. Crude annual rates of incident heat exhaustion diagnoses increased steadily during the first 3 years of the surveillance period and ranged from a low of 1.12 cases per 1,000 p-yrs in 2014 to 1.42 cases per 1,000 p-yrs in 2016 (Figure 2). Annual rates were stable during 2016–2017 and then increased 18.7% to a peak of 1.71 cases per 1,000 p-yrs in 2018. During the 5-year surveillance period, the numbers of heat exhaustion-related hospitalizations and the proportions they represented remained relatively stable (range: 49–65; 2.7%–3.4%). However, the proportions of of total heat exhaustion cases from reportable medical events increased from 29.5% in 2014 to 40.1% in 2018, while the proportions from ambulatory visits decreased from 66.3% to 57.0% during this period.
Heat illnesses by location
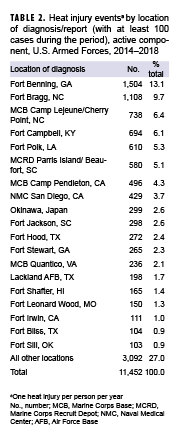
During the 5-year surveillance period, a total of 11,452 heat-related illnesses were diagnosed at more than 250 military installations and geographic locations worldwide (Table 2). Less than 8% of the total heat illness cases occurred outside of the U.S. (n=831). Four Army installations accounted for slightly more than one-third (34.2%) of all heat illnesses during the period (Fort Benning, GA [n=1,504]; Fort Bragg, NC [n=1,108]; Fort Campbell, KY [n=694]; and Fort Polk, LA [n=610]). Six other locations accounted for an additional one-quarter (24.8%) of heat illness events (Marine Corps Base Camp Lejeune/Cherry Point, NC [n=738]; Marine Corps Recruit Depot Parris Island/Beaufort, SC [n=580]; Marine Corps Base Camp Pendleton, CA [n=496]); Naval Medical Center San Diego, CA [n=429]; Okinawa, Japan [n=299]; and Fort Jackson, SC [n=298]). Of these 10 locations with the most heat illness events, 7 are located in the southeastern U.S. The 19 locations with more than 100 cases of heat illness accounted for nearly three-quarters (73.0%) of all active component cases during 2014–2018.
Heat illnesses in Iraq and Afghanistan
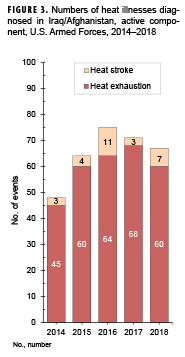
During the 5-year surveillance period, a total of 325 heat illnesses were diagnosed and treated in Iraq and Afghanistan (Figure 3). Of the total cases of heat illness, 8.6% (n=28) were diagnosed as heat stroke. Deployed service members who were affected by heat illnesses were most frequently male (n=270; 83.1%); non-Hispanic white (n=196; 60.3%); 20–24 years old (n=176; 54.2%); in the Army (n=173; 53.2%); enlisted (n=315; 96.9%); and in repair/engineering (n=109; 33.5%) or combat-specific (n=98; 30.2%) occupations (data not shown). During the surveillance period, 4 service members were medically evacuated for heat illnesses from Iraq or Afghanistan; all of the evacuations took place in the summer months (May–Sept.).
Editorial Comment
This annual update of heat illnesses among service members in the active component documented that the unadjusted annual rates of incident heat stroke diagnoses increased steadily between 2014 and 2018. The crude annual incidence rate of heat exhaustion diagnoses in 2018 represents an 18.7% increase over the 2017 rate.
There are significant limitations to this update that should be considered when interpreting the results. Similar heat-related clinical illnesses are likely managed differently and reported with different diagnostic codes at different locations and in different clinical settings. Such differences undermine the validity of direct comparisons of rates of nominal heat stroke and heat exhaustion events across locations and settings. Also, heat illnesses during training exercises and deployments that are treated in field medical facilities may not be captured in this report. In addition, it should be noted that the guidelines for mandatory reporting of heat illnesses were modified in the 2017 revision of the Armed Forces guidelines and case definitions for reportable medical events.4 In this updated version of the guidelines and case definitions, the heat injury category was removed, leaving only case classifications for heat stroke and heat exhaustion. To compensate for such possible variation in reporting, the analysis for this update, as in previous years, included cases identified in DMSS records of ambulatory care and hospitalizations using a consistent set of ICD-9/ICD-10 codes for the entire surveillance period. However, it also is important to note that the exclusion of diagnosis codes for other and unspecified effects of heat and light (formerly included within the heat illness category "other heat illnesses") in the current analysis precludes the direct comparison of numbers and rates of cases of heat exhaustion to the numbers and rates of "other heat illnesses" reported in MSMR updates prior to 2017.
As has been noted in previous MSMR heat illness updates, results indicate that a sizable proportion of cases identified through DMSS records of ambulatory visits did not prompt mandatory reports through the reporting system.20 However, this study did not directly ascertain the overlap between hospitalizations and reportable events and the overlap between reportable events and outpatient encounters. It is possible that cases of heat illness, whether diagnosed during an inpatient or outpatient encounter, were not documented as reportable medical events because treatment providers were not attentive to the criteria for reporting or because of ambiguity in interpreting the criteria (e.g., the heat illness did not result in a change in duty status or the core body temperature measured during/immediately after exertion or heat exposure was not available). Underreporting is especially concerning for cases of heat stroke because it may reflect insufficient attentiveness to the need for prompt recognition of cases of this dangerous illness and for timely intervention at the local level to prevent additional cases.
In spite of its limitations, this report documents that heat illnesses are a significant and persistent threat to both the health of U.S. military members and the effectiveness of military operations. Of all military members, the youngest and most inexperienced Marines and soldiers (particularly those training at installations in the southeastern U.S.) are at highest risk of heat illnesses, including heat stroke, exertional hyponatremia, and exertional rhabdomyolysis (see the other articles in this issue of the MSMR).
Commanders, small unit leaders, training cadre, and supporting medical personnel—particularly at recruit training centers and installations with large combat troop populations—must ensure that the military members whom they supervise and support are informed regarding the risks, preventive countermeasures (e.g., water consumption), early signs and symptoms, and first-responder actions related to heat illnesses.13–19,22 Leaders should be aware of the dangers of insufficient hydration on the one hand and excessive water intake on the other; they must have detailed knowledge of, and rigidly enforce countermeasures against, all types of heat illnesses.
Policies, guidance, and other information related to heat illness prevention and treatment among U.S. military members are available online at https://phc.amedd.army.mil/topics/discond/hipss/Pages/Heat-Related-Illness-Prevention.aspx.
Acknowledgment: The authors thank the Army Public Health Center, Aberdeen, MD, for providing data on reportable medical events of heat illnesses.
References
- Atha WF. Heat-related illness. Emerg Med Clin North Am. 2013;31(4):1097–1108.
- Simon HB. Hyperthermia. N Engl J Med. 1993;329(7):483–487.
- O'Connor FG, Sawka MN, Deuster P. Disorders due to heat and cold. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:692–693.
- Armed Forces Health Surveillance Branch in collaboration with U.S. Air Force School of Aerospace Medicine, Army Public Health Center, and Navy and Marine Corps Public Health Center. Armed Forces Reportable Medical Events: Guidelines and Case Definitions. https://health.mil/Reference-Center/Publications/2017/07/17/Armed-Forces-Reportable-Medical-Events-Guidelines. Published 17 July 2017. Accessed 11 March 2019.
- Leon LR, Bouchama A. Heat stroke. Compr Physiol. 2015;5(2):611–647.
- Epstein Y. Heat intolerance: predisposing factor or residual injury? Med Sci Sports Exerc. 1990;22(1):29–35.
- O’Connor FG, Casa DJ, Bergeron MF, et al. American College of Sports Medicine roundtable on exertional heat stroke—return to duty/return to play: conference proceedings. Curr Sports Med Rep. 2010;9(5):314–321.
- Shapiro Y, Magazanik A, Udassin R, Ben-Baruch G, Shvartz E, Shoenfeld Y. Heat intolerance in former heatstroke patients. Ann Intern Med. 1979;90(6):913–916.
- Dematte JE, O’Mara K, Buescher J, et al. Near-fatal heat stroke during the 1995 heat wave in Chicago. Ann Intern Med. 1998;129(3):173–181.
- Wallace RF, Kriebel D, Punnett L, Wegman DH, Amoroso PJ. Prior heat illness hospitalization and risk of early death. Environ Res. 2007;104(2):290–295.
- Carter R 3rd, Cheuvront SN, Williams JO, et al. Epidemiology of hospitalizations and deaths from heat illness in soldiers. Med Sci Sports Exerc. 2005;37(8):1338–1344.
- Sawka MN, Cheuvront SN, Kenefick RW. High skin temperature and hypohydration impair aerobic performance. Exp Physiol. 2012;97(3):327–332.
- Goldman RF. Introduction to heat-related problems in military operations. In Lounsbury DE, Bellamy RF, Zajtchuk R, eds. Textbook of Military Medicine: Medical Aspects of Harsh Environments, Volume 1. Washinton, DC: Office of the Surgeon General, Borden Institute; 2001:3–49.
- Sonna LA. Practical medical aspects of military operations in the heat. In Lounsbury DE, Bellamy RF, Zajtchuk R, eds. Textbook of Military Medicine: Medical Aspects of Harsh Environments, Volume 1. Washington, DC: Office of the Surgeon General, Borden Institute; 2001:293–309.
- Headquarters, Department of the Army and Air Force. Technical Bulletin, Medical, 507, Air Force Pamphlet 48-152: Heat Stress Control and Heat Casualty Management. Washington, DC: Department of the Army and Air Force; 2003. https://www.dir.ca.gov/oshsb/documents/Heat_illness_prevention_tbmed507.pdf. Accessed 11 March 2019.
- Headquarters, United States Marine Corps, Department of the Navy. Marine Corps Order 6200.1E: Marine Corps Heat Injury Prevention Program. Washington DC: Department of the Navy; 2002. http://www.marines.mil/Portals/59/Publications/MCO%206200.1E%20W%20CH%201.pdf. Accessed 11 March 2019.
- Navy Environmental Health Center. NEHCTM-OEM 6260.6A: Prevention and Treatment of Heat and Cold Stress Injuries. http://www.med.navy.mil/sites/nmcphc/Documents/nepmu-6/Environmental-Health/Disease-Prevention/Technical-Manual-NEHC-TM-OEM-6260-6A.pdf. Published June 2007. Accessed 11 March 2019.
- Webber BJ, Casa DJ, Beutler AI, Nye NS, Trueblood WE, O'Connor FG. Preventing exertional death in military trainees: recommendations and treatment algorithms from a multidisciplinary working group. Mil Med. 2016;181(4):311–318.
- Lee JK, Kenefick RW, Cheuvront SN. Novel cooling strategies for military training and operations. J Strength Cond Res. 2015;29(suppl 11):S77–S81.
- Armed Forces Health Surveillance Branch. Update: Heat injuries, active component, U.S. Armed Forces, 2017. MSMR. 2018;25(4):6–10.
- Armed Forces Health Surveillance Branch. Surveillance Case Definition. Heat Illness. March 2018. https://health.mil/Reference-Center/Publications/2017/03/01/Heat-Injuries. Accessed 11 March 2019.
- Headquarters, Department of the Army, Training and Doctrine Command. Memorandum. TRADOC Heat Illness Prevention Program 2018. 8 Jan, 2018.