By Scott C. Livingston, PhD, PT
March 9, 2020
 MHS graphic
MHS graphic
The evaluation and treatment of patients with co-occurring mild traumatic brain injury (TBI), also called concussion, and posttraumatic stress disorder (PTSD) can be a challenge for mental health care providers. Concussion and PTSD often occur together in military patients because combat-related operations can result in head trauma (physical or physiologic trauma) and psychological trauma–related experiences. The clinical assessment and differential diagnosis of patients with these co-occurring conditions can be difficult owing to the overlap of symptoms and the varied clinical course of recovery. Patients may not be thoroughly assessed for both PTSD and concussion and, therefore, may not receive comprehensive treatment or achieve optimal clinical outcomes. Additionally, there are few comorbid PTSD and mild TBI specialized treatment protocols available to providers.
The Department of Veterans Affairs (VA) and the Department of Defense (DOD) have numerous tools and resources for clinicians to help them meet the challenge of co-occurring PTSD and TBI. The 2017 VA/DOD Clinical Practice Guideline for the Management of PTSD and Acute Stress Disorder and the 2016 VA/DOD Clinical Practice Guideline for the Management of Concussion/Mild Traumatic Brain Injury provide evidence-based recommendations for patient evaluation, specific clinical tools that can be used for patient assessment, and various non-pharmacologic and pharmacologic treatment strategies.
How should a mental healthcare provider evaluate a patient with suspected PTSD and Concussion?
The signs and symptoms a patient presents with are critical elements of the differential diagnosis, but overlapping symptoms of concussion and PTSD can be confusing. Separating the unique clinical signs and symptoms of each condition from the overlapping symptoms can be useful in assessing whether the patient has comorbid PTSD and concussion. Recognizing the onset and course of clinical recovery can also be helpful; the symptoms of concussion are usually acute and resolve quickly (within days or weeks) in the vast majority of patients. On the other hand, the symptoms of PTSD last for more than a month and cause significant distress or impairment in social, occupational, or other important areas of functioning.
The VA/DOD clinical practice guidelines recommend assessing patients with symptoms attributed to concussion for psychiatric symptoms and comorbid psychiatric disorders including PTSD. Additional recommendations for patient screening in a primary care setting include using the Patient Health Questionnaire (PHQ-2 or PHQ-9), the Generalized Anxiety Disorder Scale (GAD-2 or GAD-7), and the Primary Care PTSD Screen (PC-PTSD) or PTSD Checklist (PCL).
What treatments are most effective for treating co-occurring PTSD and TBI?
- Psychosocial interventions involving exposure to trauma memory and/or cognitive restructuring have a strong clinical evidence base for treatment of PTSD.
- Cognitive behavioral therapy (CBT) demonstrates positive treatment responses in patients with mild, moderate, and severe TBI and also in patients with no history of TBI. CBT has been shown to be effective in targeting psychosocial trauma symptoms as well as decreasing symptoms of acute stress disorder (ASD), depression, and non-specific post-concussion symptoms.
- Current evidence suggests that pharmacological treatment of PTSD in patients with comorbid TBI is best approached similar to that of PTSD alone. Clinicians should be aware that potential medication side effects might increase the risk of TBI-associated problems such as cognitive deficits, sensory and balance problems, and seizures.
- Treatment recommendations for concussion are symptom based and most are based on standard clinical care rather than strong research evidence in randomized clinical trials. In general, the management of mild TBI symptoms is categorized as either non-pharmacologic (first-line treatment) or pharmacologic (second-line treatment). The concussion/mild TBI guideline provides specific recommendations for treating post-traumatic headaches, dizziness and disequilibrium, tinnitus, visual dysfunction, sleep disturbances, behavioral symptoms, cognitive symptoms, fatigue, persistent pain, hearing difficulties, smell (olfactory) deficits, and nausea.
- Because of the potential for co-occurring medical and psychiatric conditions, it is generally best to develop a collaborative care treatment strategy to address the symptoms of PTSD and concussion simultaneously.
The keys to managing service members and veterans with co-occurring PTSD and concussion is to thoroughly assess both clinical conditions and to tailor treatments according to the respective clinical practice guidelines. The overlap of concussion and PTSD symptoms can make the clinical presentation and differential diagnosis challenging, but it is important to recognize PTSD when it is present following concussion because the symptoms are often amenable to treatment. You should ensure that your patients have positive expectations for their recovery and they receive evidence-based interventions that will maximize their potential for recovery.
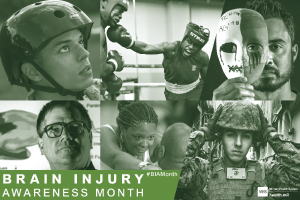
Find valuable clinical tools for providers who work with patients who have experienced concussion and information and resources for March Brain Injury Awareness Month from the Defense and Veterans Brain Injury Center.
Dr. Livingston is a contracted senior project management associate at the Psychological Health Center of Excellence. He is a subject matter expert on mild traumatic brain injury and his specialties include the assessment and management of sports-related and combat-related TBI.